| [1] |
BI ZH, WANG LX, LIAN JQ. Definition, prognostic assessment, and advances in the diagnosis and treatment of acute-on-chronic liver failure[J]. J Clin Hepatol, 2022, 38( 7): 1671- 1676. DOI: 10.3969/j.issn.1001-5256.2022.07.041. |
| [2] |
BAJAJ JS, O’LEARY JG, LAI JC, et al. Acute-on-chronic liver failure clinical guidelines[J]. Am J Gastroenterol, 2022, 117( 2): 225- 252. DOI: 10.14309/ajg.0000000000001595. |
| [3] |
MOREAU R, JALAN R, GINES P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis[J]. Gastroenterology, 2013, 144( 7): 1426- 1437. DOI: 10.1053/j.gastro.2013.02.042. |
| [4] |
SARIN SK, CHOUDHURY A, SHARMA MK, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific Association for the Study of the Liver(APASL): An update[J]. Hepatol Int, 2019, 13( 4): 353- 390. DOI: 10.1007/s12072-019-09946-3. |
| [5] |
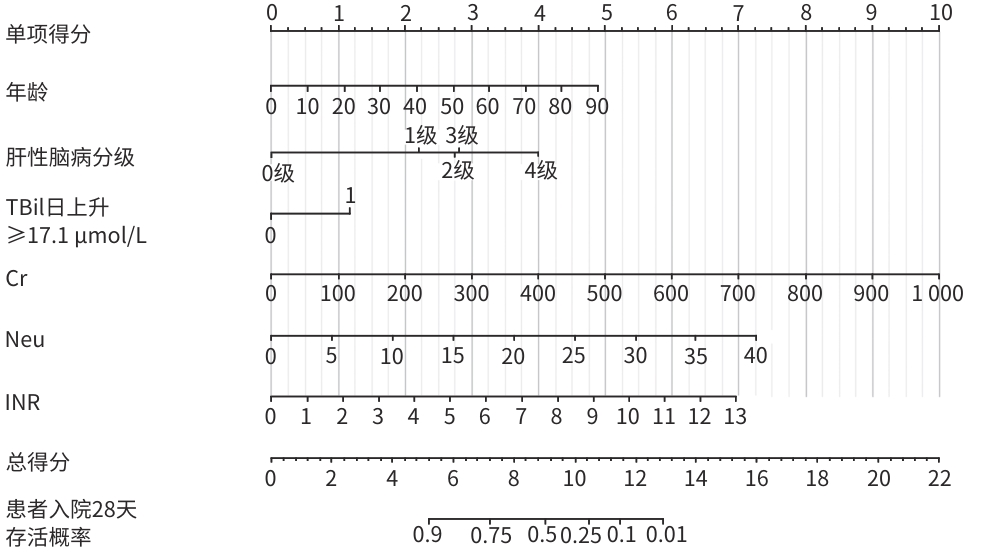
LI JQ, LIANG X, YOU SL, et al. Development and validation of a new prognostic score for hepatitis B virus-related acute-on-chronic liver failure[J]. J Hepatol, 2021, 75( 5): 1104- 1115. DOI: 10.1016/j.jhep.2021.05.026. |
| [6] |
PUGH RN, MURRAY-LYON IM, DAWSON JL, et al. Transection of the oesophagus for bleeding oesophageal varices[J]. Br J Surg, 1973, 60( 8): 646- 649. DOI: 10.1002/bjs.1800600817. |
| [7] |
MALINCHOC M, KAMATH PS, GORDON FD, et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts[J]. Hepatology, 2000, 31( 4): 864- 871. DOI: 10.1053/he.2000.5852. |
| [8] |
BIGGINS SW, KIM WR, TERRAULT NA, et al. Evidence-based incorporation of serum sodium concentration into MELD[J]. Gastroenterology, 2006, 130( 6): 1652- 1660. DOI: 10.1053/j.gastro.2006.02.010. |
| [9] |
LUCA A, ANGERMAYR B, BERTOLINI G, et al. An integrated MELD model including serum sodium and age improves the prediction of early mortality in patients with cirrhosis[J]. Liver Transpl, 2007, 13( 8): 1174- 1180. DOI: 10.1002/lt.21197. |
| [10] |
Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2024 version)[J]. J Clin Hepatol, 2024, 40( 12): 2371- 2387. DOI: 10.12449/JCH241-206.
中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2024年版)[J]. 临床肝胆病杂志, 2024, 40( 12): 2371- 2387. DOI: 10.12449/JCH241206. |
| [11] |
Chinese Society of Hepatology, Chinese Medical Association. Chinese guidelines on the management of liver cirrhosis[J]. J Clin Hepatol, 2019, 35( 11): 2408- 2425. DOI: 10.3969/j.issn.1001-5256.2019.11.006. |
| [12] |
WU TZ, LI J, SHAO L, et al. Development of diagnostic criteria and a prognostic score for hepatitis B virus-related acute-on-chronic liver failure[J]. Gut, 2018, 67( 12): 2181- 2191. DOI: 10.1136/gutjnl-2017-314641. |
| [13] |
JALAN R, YURDAYDIN C, BAJAJ JS, et al. Toward an improved definition of acute-on-chronic liver failure[J]. Gastroenterology, 2014, 147( 1): 4- 10. DOI: 10.1053/j.gastro.2014.05.005. |
| [14] |
TREBICKA J. Predisposing factors in acute-on-chronic liver failure[J]. Semin Liver Dis, 2016, 36( 2): 167- 173. DOI: 10.1055/s-0036-1583195. |
| [15] |
BAJAJ JS, O’LEARY JG, REDDY KR, et al. Survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures[J]. Hepatology, 2014, 60( 1): 250- 256. DOI: 10.1002/hep.27077. |
| [16] |
MARTIN-MATEOS R, ALVAREZ-MON M, ALBILLOS A. Dysfunctional immune response in acute-on-chronic liver failure: It takes two to tango[J]. Front Immunol, 2019, 10: 973. DOI: 10.3389/fimmu.2019.00973. |
| [17] |
WU W, SUN SS, WANG YJ, et al. Circulating neutrophil dysfunction in HBV-related acute-on-chronic liver failure[J]. Front Immunol, 2021, 12: 620365. DOI: 10.3389/fimmu.2021.620365. |
| [18] |
LEMMER P, POSPIECH JC, CANBAY A. Liver failure-future challenges and remaining questions[J]. Ann Transl Med, 2021, 9( 8): 734. DOI: 10.21037/atm-20-4968. |
| [19] |
KIM A, NIU BL, WORETA T, et al. Clinical considerations of coagulopathy in acute liver failure[J]. J Clin Transl Hepatol, 2020, 8( 4): 407- 413. DOI: 10.14218/JCTH.2020.00058. |
| [20] |
van den BOOM BP, LISMAN T. Pathophysiology and management of bleeding and thrombosis in patients with liver disease[J]. Int J Lab Hematol, 2022, 44( Suppl 1): 79- 88. DOI: 10.1111/ijlh.13856. |
| [21] |
LAI M, XU MM, WANG X, et al. Prognostic evaluation of liver transplantation for acute-on-chronic liver failure[J]. Organ Transplant, 2025, 16( 3): 482- 488. DOI: 10.12464/j.issn.1674-7445.2025002. |






 DownLoad:
DownLoad: