| [1] |
HERNAEZ R, KRAMER JR, LIU Y, et al. Prevalence and short-term mortality of acute-on-chronic liver failure: A national cohort study from the USA[J]. J Hepatol, 2019, 70( 4): 639- 647. DOI: 10.1016/j.jhep.2018.12.018. |
| [2] |
ZHANG B, DILIHUMAER ZYE, ZHANG SY, et al. Progress on pathogenesis and medical treatment of hepatitis B virus-related chronic and acute liver failure[J/CD]. Chin J Liver Dis(Electronic Version), 2023, 15( 1): 28- 33. DOI: 10.3969/j.issn.1674-7380.2023.01.005. |
| [3] |
ABDALLAH MA, KUO YF, ASRANI S, et al. Validating a novel score based on interaction between ACLF grade and MELD score to predict waitlist mortality[J]. J Hepatol, 2021, 74( 6): 1355- 1361. DOI: 10.1016/j.jhep.2020.12.003. |
| [4] |
ROLLAND Y, CZERWINSKI S, ABELLAN VAN KAN G, et al. Sarcopenia: Its assessment, etiology, pathogenesis, consequences and future perspectives[J]. J Nutr Health Aging, 2008, 12( 7): 433- 450. DOI: 10.1007/BF02982704. |
| [5] |
KIM G, KANG SH, KIM MY, et al. Prognostic value of sarcopenia in patients with liver cirrhosis: A systematic review and meta-analysis[J]. PLoS One, 2017, 12( 10): e0186990. DOI: 10.1371/journal.pone.0186990. |
| [6] |
CHAN HCN, FEI XZ, LEUNG ELY, et al. Post-discharge consequences of protein-energy malnutrition, sarcopenia, and frailty in older adults admitted to rehabilitation: A systematic review[J]. Clin Nutr ESPEN, 2023, 54: 382- 397. DOI: 10.1016/j.clnesp.2023.01.023. |
| [7] |
TANTAI XX, LIU Y, YEO YH, et al. Effect of sarcopenia on survival in patients with cirrhosis: A meta-analysis[J]. J Hepatol, 2022, 76( 3): 588- 599. DOI: 10.1016/j.jhep.2021.11.006. |
| [8] |
van VUGT JLA, ALFERINK LJM, BUETTNER S, et al. A model including sarcopenia surpasses the MELD score in predicting waiting list mortality in cirrhotic liver transplant candidates: A competing risk analysis in a national cohort[J]. J Hepatol, 2018, 68( 4): 707- 714. DOI: 10.1016/j.jhep.2017.11.030. |
| [9] |
YAO J, ZHOU XS, YUAN LL, et al. Prognostic value of the third lumbar skeletal muscle mass index in patients with liver cirrhosis and ascites[J]. Clin Nutr, 2020, 39( 6): 1908- 1913. DOI: 10.1016/j.clnu.2019.08.006. |
| [10] |
KONG M, GENG N, ZHOU Y, et al. Defining reference values for low skeletal muscle index at the L3 vertebra level based on computed tomography in healthy adults: A multicentre study[J]. Clin Nutr, 2022, 41( 2): 396- 404. DOI: 10.1016/j.clnu.2021.12.003. |
| [11] |
LIDORIKI I, SCHIZAS D, MPAILI E, et al. Associations between skeletal muscle mass index, nutritional and functional status of patients with oesophago-gastric cancer[J]. Clin Nutr ESPEN, 2019, 34: 61- 67. DOI: 10.1016/j.clnesp.2019.08.012. |
| [12] |
SARIN SK, CHOUDHURY A, SHARMA MK, et al. Acute-on-chronic liver failure: Consensus recommendations of the Asian Pacific association for the study of the liver(APASL): An update[J]. Hepatol Int, 2019, 13( 4): 353- 390. DOI: 10.1007/s12072-019-09946-3. |
| [13] |
CAREY EJ, LAI JC, WANG CW, et al. A multicenter study to define sarcopenia in patients with end-stage liver disease[J]. Liver Transpl, 2017, 23( 5): 625- 633. DOI: 10.1002/lt.24750. |
| [14] |
DURAND F, BUYSE S, FRANCOZ C, et al. Prognostic value of muscle atrophy in cirrhosis using psoas muscle thickness on computed tomography[J]. J Hepatol, 2014, 60( 6): 1151- 1157. DOI: 10.1016/j.jhep.2014.02.026. |
| [15] |
MONTANO-LOZA AJ, DUARTE-ROJO A, MEZA-JUNCO J, et al. Inclusion of sarcopenia within MELD(MELD-sarcopenia) and the prediction of mortality in patients with cirrhosis[J]. Clin Transl Gastroenterol, 2015, 6( 7): e102. DOI: 10.1038/ctg.2015.31. |
| [16] |
KAMATH PS, KIM WR. The model for end-stage liver disease(MELD)[J]. Hepatology, 2007, 45( 3): 797- 805. DOI: 10.1002/hep.21563. |
| [17] |
STEWART CA, MALINCHOC M, KIM W RAY, et al. Hepatic encephalopathy as a predictor of survival in patients with end-stage liver disease[J]. Liver Transpl, 2007, 13( 10): 1366- 1371. DOI: 10.1002/lt.21129. |
| [18] |
van VUGT JA, LEVOLGER S, de BRUIN RF, et al. Systematic review and meta-analysis of the impact of computed tomography-assessed skeletal muscle mass on outcome in patients awaiting or undergoing liver transplantation[J]. Am J Transplant, 2016, 16( 8): 2277- 2292. DOI: 10.1111/ajt.13732. |
| [19] |
MYERS RP, TANDON P, NEY M, et al. Validation of the five-variable Model for End-stage Liver Disease(5vMELD) for prediction of mortality on the liver transplant waiting list[J]. Liver Int, 2014, 34( 8): 1176- 1183. DOI: 10.1111/liv.12373. |
| [20] |
FRONTERA WR, OCHALA J. Skeletal muscle: A brief review of structure and function[J]. Calcif Tissue Int, 2015, 96( 3): 183- 195. DOI: 10.1007/s00223-014-9915-y. |
| [21] |
SAM J, NGUYEN GC. Protein-calorie malnutrition as a prognostic indicator of mortality among patients hospitalized with cirrhosis and portal hypertension[J]. Liver Int, 2009, 29( 9): 1396- 1402. DOI: 10.1111/j.1478-3231.2009.02077.x. |
| [22] |
WRIGHT G, NOIRET L, OLDE DAMINK SWM, et al. Interorgan ammonia metabolism in liver failure: The basis of current and future therapies[J]. Liver Int, 2011, 31( 2): 163- 175. DOI: 10.1111/j.1478-3231.2010.02302.x. |
| [23] |
|
| [24] |
LI JH, YAO J, YUAN LL. Association between sarcopenia and hepatic encephalopathy and advances in diagnosis and treatment[J]. J Clin Hepatol, 2020, 36( 6): 1412- 1414. DOI: 10.3969/j.issn.1001-5256.2020.06.049. |
| [25] |
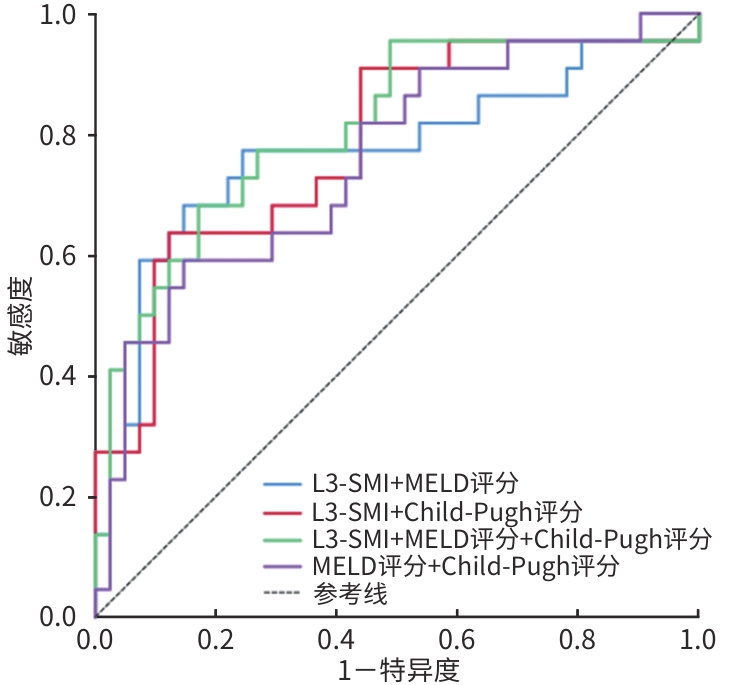
PENG H, ZHANG Q, LUO L, et al. A prognostic model of acute-on-chronic liver failure based on sarcopenia[J]. Hepatol Int, 2022, 16( 4): 964- 972. DOI: 10.1007/s12072-022-10363-2. |








 DownLoad:
DownLoad: