肝衰竭背景下肝脏再生的分子机制及其治疗潜力
DOI: 10.12449/JCH251231
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:朱先茹负责论文的思路设计及论文的撰写;任锋负责文稿审阅、经费支持。
Molecular mechanisms of liver regeneration and its therapeutic potential in the context of liver failure
-
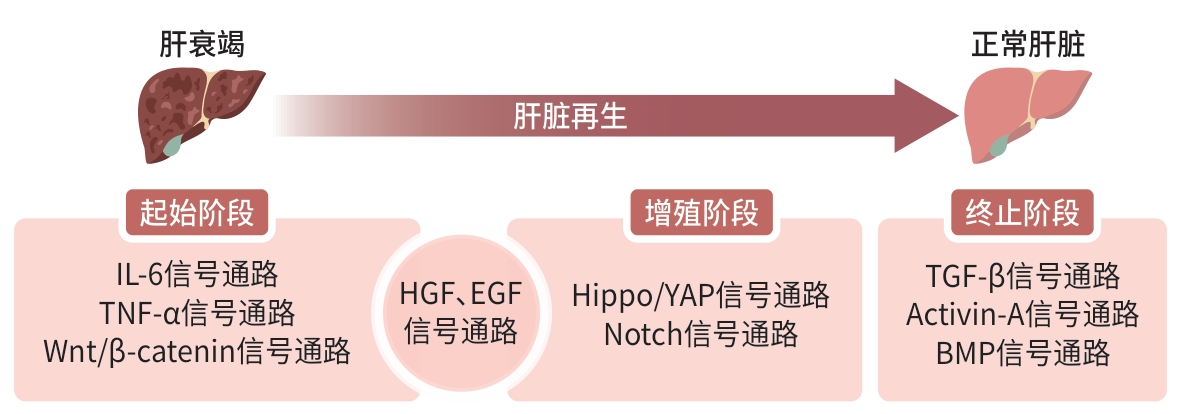
摘要: 肝衰竭是一类由多种致病因素导致肝细胞坏死速度超过其自我修复能力的临床综合征,对人类健康构成严重威胁。由于肝衰竭发病机制复杂,发病率和死亡率高,且缺乏特效疗法,目前仍是临床治疗热点及难点。肝脏再生作为肝脏应对损伤的重要机制,是肝衰竭患者救治成功的关键因素之一,在肝衰竭的发病和预后中发挥至关重要的作用。肝脏再生过程复杂,涉及多种细胞因子和转录因子相互作用,通过激活不同的信号通路,共同推动肝细胞增殖与组织修复。本文系统综述了肝脏再生在肝衰竭中的分子机制,强调了IL-6、TNF-α和HGF等细胞因子以及相关信号通路在调节肝细胞增殖和组织修复中的关键作用,以及肝衰竭背景下肝脏再生的治疗潜力,为进一步开展肝衰竭中的肝脏再生基础研究提供参考。Abstract: Liver failure is a clinical syndrome in which the speed of hepatocyte necrosis exceeds the self-repair capacity of the liver and is caused by various pathogenic factors, posing a serious threat to human health. Due to the complex pathogenesis, high incidence rate, and high mortality rate of liver failure and a lack of effective treatment methods, the treatment of liver failure remains a global challenge and a difficult issue. As an important mechanism by which the liver responds to liver injury, liver regeneration is one of the key factors for successful treatment of liver failure patients and plays a vital role in the development and prognosis of liver failure. Liver regeneration is an extremely complex biological process involving multiple cytokines and transcription factors, which jointly promote hepatocyte proliferation and tissue repair by activating various signaling pathways. This article systematically reviews the molecular mechanism of liver regeneration in liver failure, emphasizes the key role of cytokines (such as interleukin-6, tumor necrosis factor-α, and hepatocyte growth factor) and related signaling pathways in regulating hepatocyte proliferation and tissue repair, and explores the therapeutic potential of liver regeneration in the context of liver failure, in order to provide a reference for the basic research on liver regeneration in liver failure.
-
Key words:
- Liver Failure /
- Liver Regeneration /
- Signaling Pathway
-
[1] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association; Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2024 version)[J]. J Clin Hepatol, 2024, 40( 12): 2371- 2387. DOI: 10.12449/JCH241206.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组. 肝衰竭诊治指南(2024年版)[J]. 临床肝胆病杂志, 2024, 40( 12): 2371- 2387. DOI: 10.12449/JCH241206. [2] MA X, HUANG TD, CHEN XZ, et al. Molecular mechanisms in liver repair and regeneration: From physiology to therapeutics[J]. Signal Transduct Target Ther, 2025, 10( 1): 63. DOI: 10.1038/s41392-024-02104-8. [3] van der MERWE S, CHOKSHI S, BERNSMEIER C, et al. The multifactorial mechanisms of bacterial infection in decompensated cirrhosis[J]. J Hepatol, 2021, 75( Suppl 1): S82- S100. DOI: 10.1016/j.jhep.2020.11.029. [4] LI WP, LI L, HUI LJ. Cell plasticity in liver regeneration[J]. Trends Cell Biol, 2020, 30( 4): 329- 338. DOI: 10.1016/j.tcb.2020.01.007. [5] FERNÁNDEZ J, ACEVEDO J, WIEST R, et al. Bacterial and fungal infections in acute-on-chronic liver failure: Prevalence, characteristics and impact on prognosis[J]. Gut, 2018, 67( 10): 1870- 1880. DOI: 10.1136/gutjnl-2017-314240. [6] BLAKE MJ, STEER CJ. Liver regeneration in acute on chronic liver failure[J]. Clin Liver Dis, 2023, 27( 3): 595- 616. DOI: 10.1016/j.cld.2023.03.005. [7] DI-IACOVO N, PIERONI S, PIOBBICO D, et al. Liver regeneration and immunity: A tale to tell[J]. Int J Mol Sci, 2023, 24( 2): 1176. DOI: 10.3390/ijms24021176. [8] CAMPANA L, ESSER H, HUCH M, et al. Liver regeneration and inflammation: From fundamental science to clinical applications[J]. Nat Rev Mol Cell Biol, 2021, 22( 9): 608- 624. DOI: 10.1038/s41580-021-00373-7. [9] YU W, ZHANG LJ, LU Y, et al. Role of STAT3 in hepatocyte regeneration after acetaminophen-induced hepatocellular injury in mice[J]. J Clin Hepatol, 2021, 37( 4): 857- 862. DOI: 10.3969/j.issn.1001-5256.2021.04.026.余旺, 章礼久, 路燕, 等. STAT3在对乙酰氨基酚所致小鼠肝损伤后肝细胞再生中的作用[J]. 临床肝胆病杂志, 2021, 37( 4): 857- 862. DOI: 10.3969/j.issn.1001-5256.2021.04.026. [10] ENGELMANN C, MEHTA G, TACKE F. Regeneration in acute-on-chronic liver failure-the phantom lost its camouflage[J]. J Hepatol, 2020, 72( 4): 610- 612. DOI: 10.1016/j.jhep.2020.01.003. [11] HAFEZ MM, AL-HARBI NO, AL-HOSHANI AR, et al. Hepato-protective effect of rutin via IL-6/STAT3 pathway in CCl4-induced hepatotoxicity in rats[J]. Biol Res, 2015, 48( 1): 30. DOI: 10.1186/s40659-015-0022-y. [12] XIANG XG, FENG DC, HWANG S, et al. Interleukin-22 ameliorates acute-on-chronic liver failure by reprogramming impaired regeneration pathways in mice[J]. J Hepatol, 2020, 72( 4): 736- 745. DOI: 10.1016/j.jhep.2019.11.013. [13] LIN YP, LIU XP, LUO YB, et al. The relationship between the Wnt signaling pathway and liver regeneration and its role in liver diseases[J]. J Clin Hepatol, 2024, 40( 5): 1050- 1056. DOI: 10.12449/JCH240529.林玉培, 刘晓萍, 罗银冰, 等. Wnt信号通路与肝再生的关系及其在肝脏疾病中的作用[J]. 临床肝胆病杂志, 2024, 40( 5): 1050- 1056. DOI: 10.12449/JCH240529. [14] YIN YZ, KONG DF, HE K, et al. Aurora kinase A regulates liver regeneration through macrophages polarization and Wnt/β-catenin signalling[J]. Liver Int, 2022, 42( 2): 468- 478. DOI: 10.1111/liv.15094. [15] LIU H, GAO X, ZHANG W, et al. DDX17-Mediated upregulation of CXCL8 promotes hepatocellular carcinoma progression via co-activating β-catenin/NF-κB complex[J]. Int J Biol Sci, 2025, 21( 3): 1342- 1360. DOI: 10.7150/ijbs.104165. [16] SUN TL, ANNUNZIATO S, BERGLING S, et al. ZNRF3 and RNF43 cooperate to safeguard metabolic liver zonation and hepatocyte proliferation[J]. Cell Stem Cell, 2021, 28( 10): 1822- 1837.e10. DOI: 10.1016/j.stem.2021.05.013. [17] LIU Q, WANG SY, FU J, et al. Liver regeneration after injury: Mechanisms, cellular interactions and therapeutic innovations[J]. Clin Transl Med, 2024, 14( 8): e1812. DOI: 10.1002/ctm2.1812. [18] ROBARTS DR, MCGREAL SR, UMBAUGH DS, et al. Regulation of liver regeneration by hepatocyte O-GlcNAcylation in mice[J]. Cell Mol Gastroenterol Hepatol, 2022, 13( 5): 1510- 1529. DOI: 10.1016/j.jcmgh.2022.01.014. [19] ZHU JN, KOLTSOVA EK. Two faces of NOTCH1 in liver cancer and immunotherapy[J]. Cancer Discov, 2025, 15( 3): 452- 454. DOI: 10.1158/2159-8290.CD-24-1883. [20] VERBOVEN E, MOYA IM, SANSORES-GARCIA L, et al. Regeneration defects in Yap and taz mutant mouse livers are caused by bile duct disruption and cholestasis[J]. Gastroenterology, 2021, 160( 3): 847- 862. DOI: 10.1053/j.gastro.2020.10.035. [21] HENG BC, ZHANG XH, AUBEL D, et al. An overview of signaling pathways regulating YAP/TAZ activity[J]. Cell Mol Life Sci, 2021, 78( 2): 497- 512. DOI: 10.1007/s00018-020-03579-8. [22] YI M, LI TY, NIU MK, et al. TGF-β: A novel predictor and target for anti-PD-1/PD-L1 therapy[J]. Front Immunol, 2022, 13: 1061394. DOI: 10.3389/fimmu.2022.1061394. [23] WANG SY, WANG X, SHAN YR, et al. Region-specific cellular and molecular basis of liver regeneration after acute pericentral injury[J]. Cell Stem Cell, 2024, 31( 3): 341- 358. e 7. DOI: 10.1016/j.stem.2024.01.013. [24] ZHANG C, WEI WJ, TU S, et al. Upregulation of CYR61 by TGF-β and YAP signaling exerts a counter-suppression of hepatocellular carcinoma[J]. J Biol Chem, 2024, 300( 4): 107208. DOI: 10.1016/j.jbc.2024.107208. [25] YU M, WANG JN, ZHANG X, et al. The mechanism of YAP/TAZ transactivation and dual targeting for cancer therapy[J]. Nat Commun, 2025, 16( 1): 3855. DOI: 10.1038/s41467-025-59309-w. [26] ZHANG W, ZHU LJ, FANG F, et al. Activin A plays an essential role in migration and proliferation of hepatic stellate cells via Smad3 and calcium signaling[J]. Sci Rep, 2024, 14( 1): 20419. DOI: 10.1038/s41598-024-71304-7. [27] PARROW NL, FLEMING RE. BMPs and iron: The ins and outs[J]. Blood, 2025, 145( 6): 557- 558. DOI: 10.1182/blood.2024027052. [28] CUI BY, YANG L, ZHAO YY, et al. HOXA13 promotes liver regeneration through regulation of BMP-7[J]. Biochem Biophys Res Commun, 2022, 623: 23- 31. DOI: 10.1016/j.bbrc.2022.07.018. [29] MA C, WANG C, ZHANG YF, et al. Phillygenin inhibited M1 macrophage polarization and reduced hepatic stellate cell activation by inhibiting macrophage exosomal miR-125b-5p[J]. Biomed Pharmacother, 2023, 159: 114264. DOI: 10.1016/j.biopha.2023.114264. [30] ABDEL HALIM AS, RUDAYNI HA, AHMAD CHAUDHARY A, et al. microRNAs: Small molecules with big impacts in liver injury[J]. J Cell Physiol, 2023, 238( 1): 32- 69. DOI: 10.1002/jcp.30908. [31] MUNAKATA C, FUCHIGAMI Y, HIROISHI S, et al. Evaluation of miR-122 to predict high dose acetaminophen-induced liver injury in mice: The combination uses of 5-fluorouracil[J]. Biol Pharm Bull, 2018, 41( 11): 1732- 1735. DOI: 10.1248/bpb.b18-00504. [32] WESLEY BT, ROSS ADB, MURARO D, et al. Single-cell atlas of human liver development reveals pathways directing hepatic cell fates[J]. Nat Cell Biol, 2022, 24( 10): 1487- 1498. DOI: 10.1038/s41556-022-00989-7. [33] ZHANG CY, YE BY, WEI JJ, et al. miR-199a-5p regulates rat liver regeneration and hepatocyte proliferation by targeting TNF-α TNFR1/TRADD/CASPASE8/CASPASE3 signalling pathway[J]. Artif Cells Nanomed Biotechnol, 2019, 47( 1): 4110- 4118. DOI: 10.1080/21691401.2019.1683566. [34] HUANG CY, LI WX, JIANG S, et al. Application of mesenchymal stem cell-derived exosomes in liver regeneration[J/OL]. Chin J Transplatation Electron Ed, 2025, 19( 4): 268- 273. DOI: 10.3877/cma.j.issn.1674-3903.2025.04.010.黄淳雨, 李文馨, 蒋上, 等. 间充质干细胞来源外泌体在肝再生领域的应用[J/OL]. 中华移植杂志(电子版), 2025, 19( 4): 268- 273. DOI: 10. 3877/cma.j.issn.1674-3903.2025.04.010. [35] KIM J, LEE SK, JEONG SY, et al. Multifaceted action of stem cell-derived extracellular vesicles for nonalcoholic steatohepatitis[J]. J Control Release, 2023, 364: 297- 311. DOI: 10.1016/j.jconrel.2023.10.045. [36] LI Y, LU LG, CAI XB. Liver regeneration and cell transplantation for end-stage liver disease[J]. Biomolecules, 2021, 11( 12): 1907. DOI: 10.3390/biom11121907. [37] YADAV P, SINGH SK, RAJPUT S, et al. Therapeutic potential of stem cells in regeneration of liver in chronic liver diseases: Current perspectives and future challenges[J]. Pharmacol Ther, 2024, 253: 108563. DOI: 10.1016/j.pharmthera.2023.108563. [38] WANG LF, ZHANG Z, XU RN, et al. Human umbilical cord mesenchymal stem cell transfusion in immune non-responders with AIDS: A multicenter randomized controlled trial[J]. Signal Transduct Target Ther, 2021, 6( 1): 217. DOI: 10.1038/s41392-021-00607-2. -



 PDF下载 ( 652 KB)
PDF下载 ( 652 KB)

 下载:
下载:


