C反应蛋白-白蛋白-淋巴细胞指数、C反应蛋白与淋巴细胞比值和C反应蛋白与血清钙比值对急性胰腺炎患者病情程度及预后的评估价值
DOI: 10.12449/JCH251222
Value of C-reactive protein-albumin-lymphocyte index, C-reactive protein-to-lymphocyte ratio, and C-reactive protein-to-serum calcium ratio in evaluating the severity and prognosis of patients with acute pancreatitis
-
摘要:
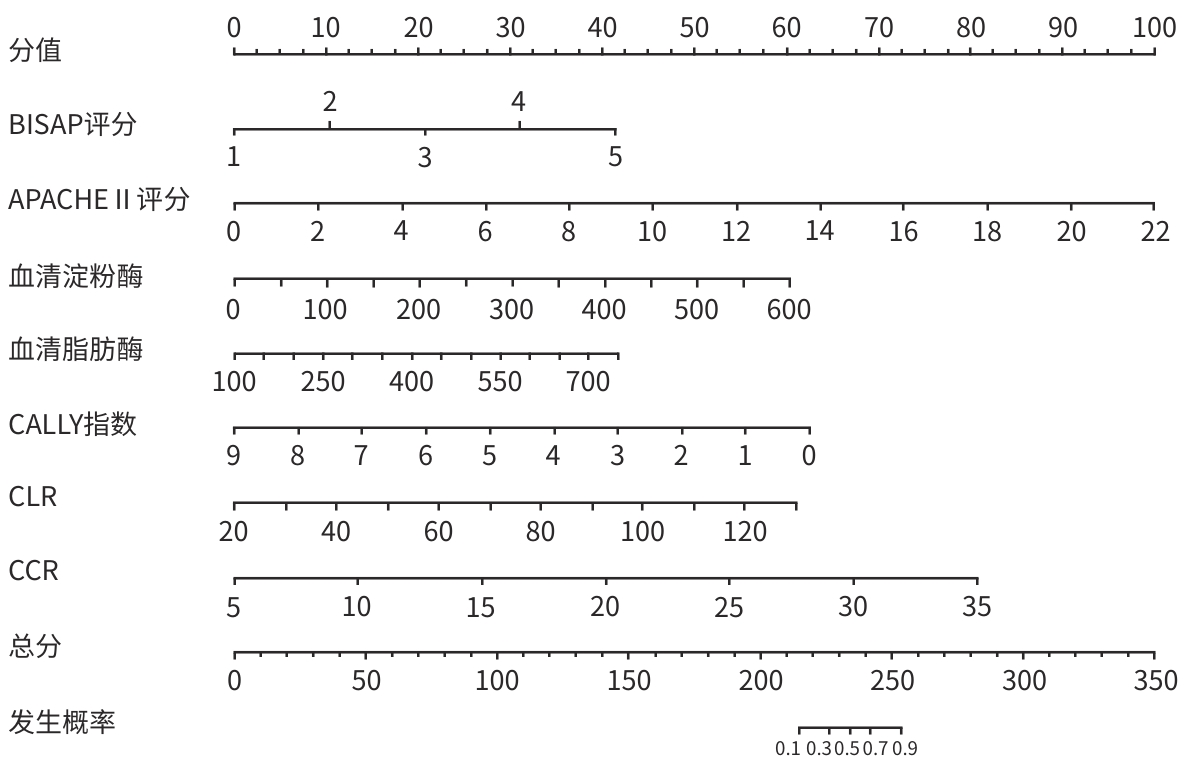
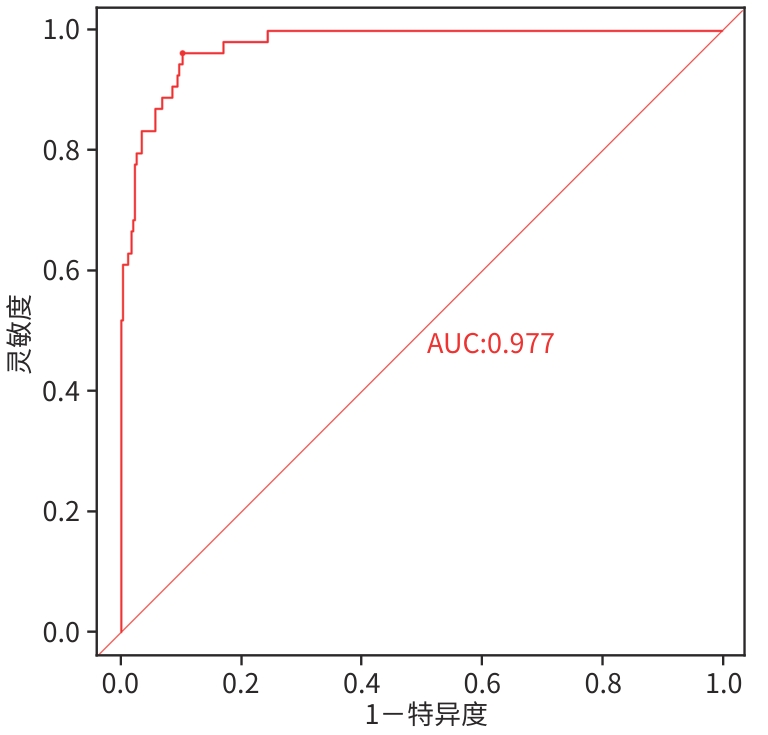
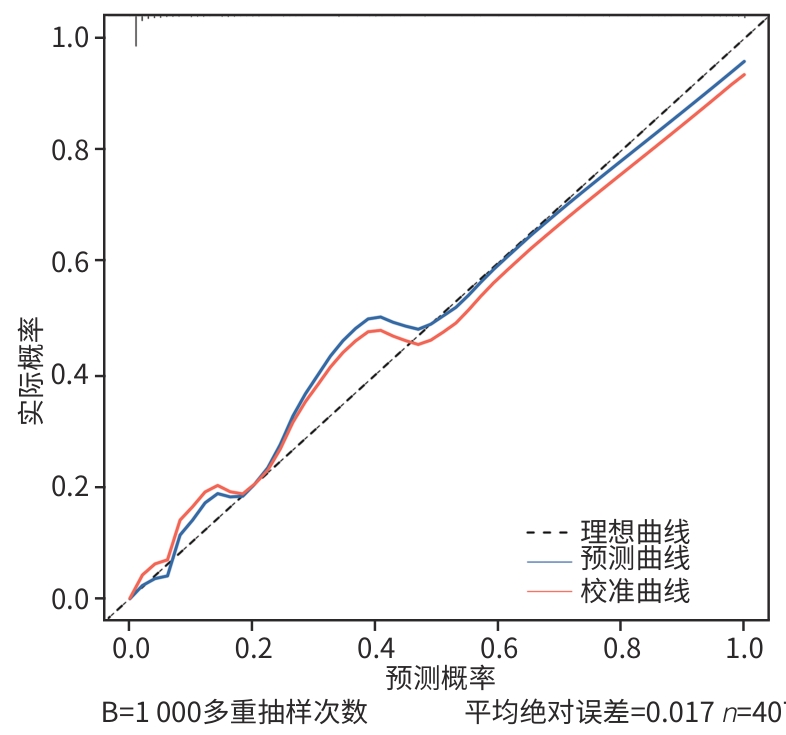
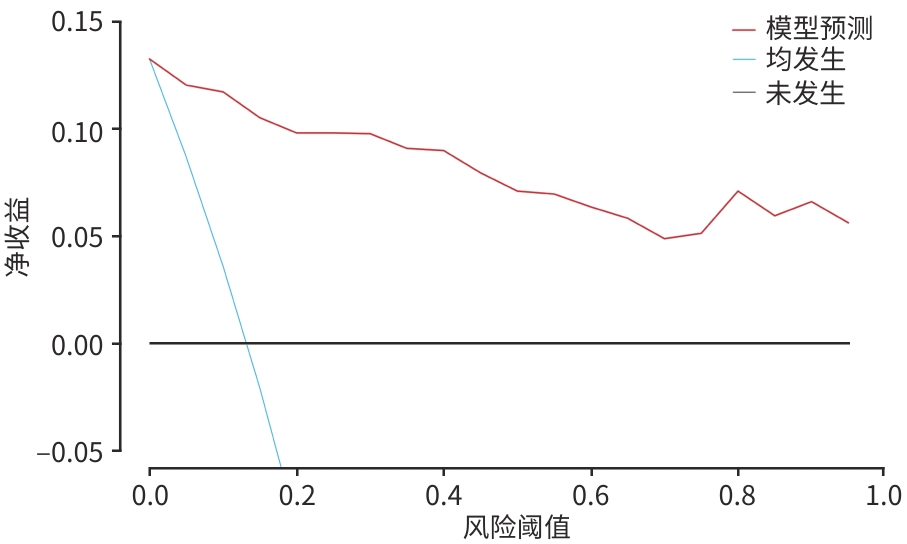
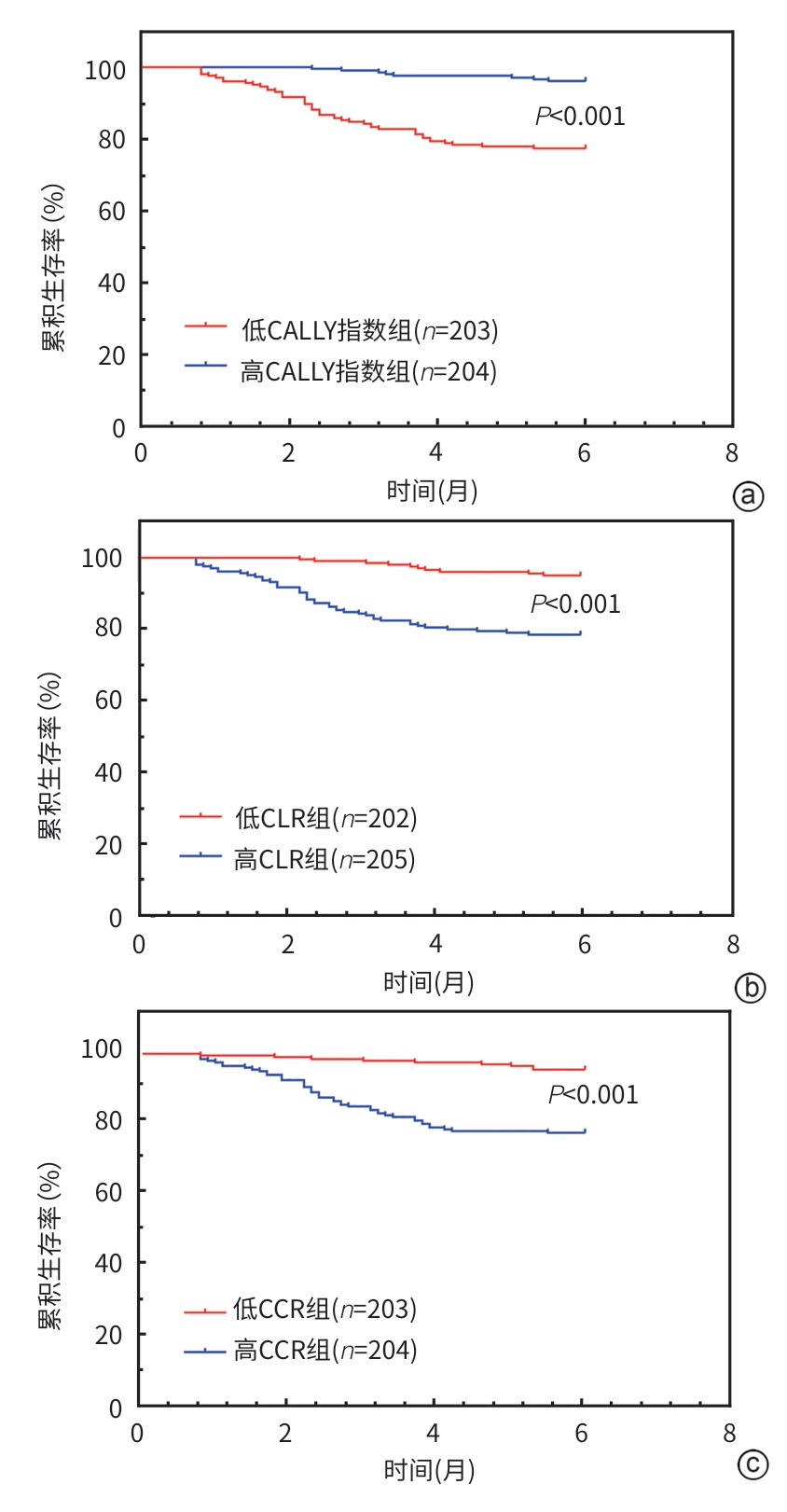
目的 探讨C反应蛋白-白蛋白-淋巴细胞(CALLY)指数、C反应蛋白与淋巴细胞比值(CLR)和C反应蛋白与血清钙比值(CCR)与急性胰腺炎(AP)患者病情严重程度及预后的关系,并构建预后预测模型,为临床评估病情及判断预后提供参考。 方法 选取2021年6月—2024年6月在苏州大学附属第一医院诊治的407例AP患者为研究对象,根据2012年修订版亚特兰大分类标准和6个月内的预后情况,将患者分别分为轻症组(n=146)、中症组(n=137)和重症组(n=124),以及预后不良组(n=54)和预后良好组(n=353)。收集患者的临床资料,并计算CALLY指数、CLR和CCR。计量资料2组间比较采用成组t检验,3组间比较采用单因素方差分析。计数资料组间比较采用χ2检验。Pearson相关性分析CALLY指数、CLR和CCR与AP患者病情程度及预后的相关性,Cox回归分析AP患者预后不良的影响因素。Kaplan-Meier生存曲线分析CALLY指数、CLR和CCR对AP患者总生存期(OS)的影响,采用R软件基于多因素Cox回归分析筛选出的危险因素构建预测AP患者预后不良的列线图模型,并绘制受试者操作特征曲线分析各独立因素单独及联合对AP患者预后不良的预测价值。 结果 轻症组、中症组、重症组3组及预后良好组、预后不良组2组患者的CT严重指数(CTSI)评分、严重程度床边指数(BISAP)评分、急性生理学与慢性健康状况评价Ⅱ(APACHE Ⅱ)评分、血尿素氮、血清乳酸、血清淀粉酶、血清脂肪酶、CALLY指数、CLR和CCR比较,差异均有统计学意义(P值均<0.05)。Pearson相关性分析显示,CALLY指数与AP病情严重程度和预后呈负相关(rs=-0.134、-0.280),而CLR和CCR则呈正相关(rs=0.213~0.345)(P值均<0.05)。Cox回归分析证实,高BISAP评分(HR=2.246,95%CI:1.412~3.570)、高APACHE Ⅱ评分(HR=1.202,95%CI:1.089~1.327)、高血清淀粉酶水平(HR=1.004,95%CI:1.001~1.007)、高血清脂肪酶(HR=1.005,95%CI:1.002~1.008)、低CALLY指数(HR=0.536,95%CI:0.397~0.724)、高CLR(HR=1.033,95%CI:1.011~1.055)和高CCR(HR=1.144,95%CI:1.062~1.232)是AP预后不良的独立危险因素(P值均<0.05)。Kaplan-Meier生存曲线分析显示,低CALLY指数患者中位OS短于高CALLY指数患者(Log-rank χ2=31.934,P<0.001);高CLR、高CCR患者中位OS分别短于低CLR、低CCR患者(Log-rank χ2=34.201、28.023,P值均<0.001)。基于多因素分析构建的列线图模型展现出优异的预测效能(曲线下面积=0.977),显著优于各单项指标(P值均<0.05),当取Cut-off值0.107时,其灵敏度和特异度分别达0.963和0.898。内部验证证实模型稳定性良好(C-index=0.954),决策分析显示其具有理想的临床适用性。 结论 CALLY指数、CLR和CCR与AP患者病情严重程度及预后具有相关性。高BISAP评分、高APACHE Ⅱ评分、高血清酶水平、低CALLY指数、高CLR和高CCR是预后不良的独立危险因素,基于多因素构建的列线图模型具有较高的预测效能,能够实现对AP患者预后的早期、精准预测,为临床开展个体化干预和动态风险评估提供实用工具。 Abstract:Objective To investigate the association of C-reactive protein-albumin-lymphocyte (CALLY) index, C-reactive protein-to-lymphocyte ratio (CLR), and C-reactive protein-to-serum calcium ratio (CCR) with the severity and prognosis of patients with acute pancreatitis (AP), to construct a prognosis prediction model, and to provide a reference for clinical assessment of severity and prognosis. Methods A total of 407 AP patients who were diagnosed and treated in The First Affiliated Hospital of Soochow University from June 2021 to June 2024 were enrolled as subjects, and according to the 2012 revised edition of Atlanta classification standard and the prognosis within 6 months, the patients were divided into mild disease group with 146 patients, moderate disease group with 137 patients, and severe disease group with 124 patients, as well as into poor prognosis group with 54 patients and good prognosis group with 353 patients. Clinical data were collected from all subjects, and CALLY index, CLR, and CCR values were calculated. The independent samples t-test was used for comparison of continuous data between two groups, and a one-way analysis of variance was used for comparison between three groups; the chi-square test was used for comparison of categorical data between groups. A Pearson correlation analysis was used to investigate the correlation of CALLY index, CLR, and CCR with the severity and prognosis of AP patients, and the Cox regression analysis was used to identify the influencing factors for poor prognosis of AP patients. The Kaplan-Meier survival curve was used to analyze the influence of CALLY index, CLR, and CCR on the overall survival (OS) of AP patients; R software was used to construct a nomogram model for predicting poor prognosis of AP patients based on risk factors identified by the multivariate Cox regression analysis. The receiver operating characteristic (ROC) curve was plotted to analyze the value of each independent factor used alone or in combination in predicting the poor prognosis of AP patients. Results There were significant differences between the mild, moderate, and severe disease groups in Computed Tomography Severity Index, Bedside Index for Severity in Acute Pancreatitis (BISAP) score, Acute Physiology and Chronic Health Evaluation Ⅱ(APACHE Ⅱ) score, blood urea nitrogen, serum lactic acid, serum amylase, serum lipase, CALLY index, CLR, and CCR, and there were also significant differences in these indicators between the good prognosis group and the poor prognosis group (all P<0.05). The Pearson correlation analysis showed that CALLY index was negatively correlated with the severity and prognosis of AP (rs =-0.134 and -0.280,both P<0.05), while CLR and CCR were positively correlated with the severity and prognosis of AP (rs =0.213 — 0.345,all P<0.05). The Cox regression analysis confirmed that high BISAP score(HR=2.246,95%CI:1.412 — 3.570), high APACHE Ⅱ score(HR=1.202,95%CI:1.089 — 1.327), high serum amylase level(HR=1.004,95%CI:1.001 — 1.007),high serum lipase level(HR=1.005,95%CI:1.002 — 1.008), low CALLY inde(HR=0.536,95%CI:0.397 — 0.724), high CLR(HR=1.033,95%CI:1.011 — 1.055), and high CCR (HR=1.144,95%CI:1.062 — 1.232)were independent risk factors for the poor prognosis of AP (all P<0.05). The Kaplan-Meier survival curve analysis showed that the patients with low CALLY index had a shorter median OS than those with high CALLY index (Log-rank χ2=31.934, P<0.001), and the patients with high CLR and CCR had a significantly shorter median OS than those with low CLR and CCR, respectively (Log-rank χ2=34.201 and 28.023, both P<0.001). The nomogram model constructed based on the multivariate analysis showed excellent predictive efficiency, with an area under the ROC curve (AUC) of 0.977, which was significantly better than the AUC of each indicator used alone (P<0.05), when the cut-off value is 0.107,the sensitivity and specificity of the nomogram model reached 0.963 and 0.898, respectively. Internal validation confirmed that the model had good stability, with a C-index of 0.954, and the decision curve analysis showed that it had satisfactory clinical applicability. Conclusion CALLY index, CLR, and CCR are correlated with the severity and prognosis of AP patients. High BISAP score, high APACHE II score, high serum enzyme level, low CALLY index, high CLR, and high CCR are independent risk factors for poor prognosis, and the nomogram model constructed based on multiple factors has high predictive efficiency and can achieve early accurate prediction of the prognosis of AP patients, thereby providing a practical tool for individualized intervention and dynamic risk assessment in clinical practice. -
Key words:
- Pancreatitis /
- Patient Acuity /
- Prognosis
-
表 1 不同病情程度患者的临床资料比较
Table 1. Comparison of clinical data of patients with different degrees of disease
指标 轻症组(n=146) 中症组(n=137) 重症组(n=124) 统计值 P值 性别[例(%)] χ2=0.924 0.630 男 67(45.89) 68(49.64) 64(51.61) 女 79(54.11) 69(50.36) 60(48.39) 年龄[例(%)] χ2=3.801 0.150 <60岁 87(59.59) 66(48.18) 69(55.65) ≥60岁 59(40.41) 71(51.82) 55(44.35) BMI(kg/m2) 23.63±2.73 24.13±2.70 23.67±2.82 F=1.394 0.249 糖尿病[例(%)] χ2=0.220 0.896 无 134(91.78) 127(92.70) 113(91.13) 有 12(8.22) 10(7.30) 11(8.87) 高血压[例(%)] χ2=1.681 0.432 无 133(91.10) 123(89.78) 107(86.29) 有 13(8.90) 14(10.22) 17(13.71) 病因[例(%)] χ2=4.795 0.309 高脂血症 41(28.08) 29(21.17) 29(23.39) 胆源性 79(54.11) 70(51.09) 68(54.84) 酒精性 26(17.81) 38(27.74) 27(21.77) CTSI评分(分) 5.45±1.07 5.95±0.86 5.98±0.92 F=13.856 <0.001 BISAP评分(分) 2.52±0.70 2.95±0.67 3.11±0.69 F=27.447 <0.001 APACHE Ⅱ评分(分) 8.34±2.11 9.96±3.02 11.55±3.19 F=44.633 <0.001 空腹血糖(mmol/L) 7.92±2.39 7.68±2.39 7.99±2.49 F=0.589 0.555 WBC(×109/L) 14.31±4.59 14.99±4.29 14.79±4.49 F=0.879 0.416 BUN(mmol/L) 5.45±0.84 5.66±0.91 5.83±1.01 F=5.921 0.003 血清乳酸(mmol/L) 9.72±1.45 9.84±1.58 10.37±1.54 F=6.917 0.001 Cr(μmol/L) 79.66±12.20 78.27±10.61 79.34±11.36 F=0.567 0.568 TBil(mg/dL) 2.94±0.98 3.01±0.98 3.06±1.03 F=0.472 0.624 血清淀粉酶(U/L) 219.03±77.48 235.52±98.08 308.81±100.46 F=35.204 <0.001 血清脂肪酶(U/L) 362.38±72.35 374.31±98.77 438.34±103.10 F=25.886 <0.001 CALLY指数 4.67±1.13 4.77±1.24 4.21±1.13 F=8.396 <0.001 CLR 63.30±11.39 63.31±10.52 71.14±14.57 F=17.850 <0.001 CCR 15.28±3.51 17.10±2.92 18.75±4.18 F=32.180 <0.001 注:BMI,体重指数;CTSI,CT严重指数;BISAP,严重程度床边指数;APACHE Ⅱ,急性生理学与慢性健康状况评价Ⅱ;WBC,白细胞计数;BUN,血尿素氮;Cr,肌酐;TBil,总胆红素;CALLY,C反应蛋白-白蛋白-淋巴细胞;CLR,C-反应蛋白与淋巴细胞比值;CCR,C-反应蛋白与血清钙比值。
表 2 预后不良组和预后良好组的临床资料比较
Table 2. Comparison of clinical data between the poor prognosis group and the good prognosis group
指标 预后良好组(n=353) 预后不良组(n=54) 统计值 P值 性别[例(%)] χ2=0.218 0.641 男 171(48.44) 28(51.85) 女 182(51.56) 26(48.15) 年龄[例(%)] χ2=0.026 0.873 <60岁 192(54.39) 30(55.56) ≥60岁 161(45.61) 24(44.44) BMI(kg/m2) 23.78±2.75 24.03±2.81 t=-0.623 0.533 糖尿病[例(%)] χ2=1.970 0.160 无 327(92.63) 47(87.04) 有 26(7.37) 7(12.96) 高血压[例(%)] χ2=2.214 0.137 无 318(90.08) 45(83.33) 有 35(9.92) 9(16.67) 病因[例(%)] χ2=0.756 0.685 高脂血症 88(24.93) 11(20.37) 胆源性 188(53.26) 29(53.70) 酒精性 77(21.81) 14(25.93) CTSI评分(分) 5.74±1.01 6.04±0.78 t=-2.071 0.039 BISAP评分(分) 2.76±0.69 3.37±0.73 t=-5.925 <0.001 APACHE Ⅱ评分(分) 9.32±2.61 13.41±3.52 t=-8.211 <0.001 空腹血糖(mmol/L) 7.82±2.37 8.09±2.69 t=-0.763 0.446 WBC(×109/L) 14.59±4.43 15.33±4.65 t=-1.137 0.256 BUN(mmol/L) 5.58±0.87 6.03±1.16 t=-2.783 0.007 血清乳酸(mmol/L) 9.89±1.51 10.43±1.71 t=-2.409 0.016 Cr(μmol/L) 78.91±11.57 80.33±10.33 t=-0.851 0.395 TBil(mg/dL) 2.98±0.99 3.16±1.03 t=-1.310 0.191 血清淀粉酶(U/L) 236.94±89.95 349.98±103.63 t=-8.422 <0.001 血清脂肪酶(U/L) 376.33±86.50 475.91±117.38 t=-7.478 <0.001 CALLY指数 4.69±1.19 3.79±0.81 t=7.061 <0.001 CLR 63.99±11.31 76.85±15.37 t=-5.907 <0.001 CCR 16.36±3.35 20.87±4.39 t=-7.241 <0.001 注:BMI,体重指数;CTSI,CT严重指数;BISAP,严重程度床边指数;APACHE Ⅱ,急性生理学与慢性健康状况评价Ⅱ;WBC,白细胞计数;BUN,血尿素氮;Cr,肌酐;TBil,总胆红素;CALLY,C反应蛋白-白蛋白-淋巴细胞;CLR,C-反应蛋白与淋巴细胞比值;CCR,C-反应蛋白与血清钙比值。
表 3 多因素Cox回归分析AP患者预后不良的独立危险因素
Table 3. Multivariate Cox regression analysis of independent risk factors of poor prognosis in AP patients
变量 β值 SE Wald P值 HR(95%CI) CTSI评分 0.184 0.164 1.265 0.261 1.202(0.872~1.658) BISAP评分 0.809 0.237 11.691 0.001 2.246(1.412~3.570) APACHE Ⅱ评分 0.184 0.050 13.386 <0.001 1.202(1.089~1.327) BUN 0.175 0.158 1.217 0.270 1.191(0.873~1.624) 血清乳酸 0.039 0.091 0.183 0.669 1.040(0.870~1.242) 血清淀粉酶 0.004 0.002 6.290 0.012 1.004(1.001~1.007) 血清脂肪酶 0.005 0.002 9.003 0.003 1.005(1.002~1.008) CALLY指数 -0.623 0.153 16.515 <0.001 0.536(0.397~0.724) CLR 0.032 0.011 8.842 0.003 1.033(1.011~1.055) CCR 0.134 0.038 12.662 <0.001 1.144(1.062~1.232) 注:CTSI,CT严重指数;BISAP,严重程度床边指数;APACHE Ⅱ,急性生理学与慢性健康状况评价Ⅱ;BUN,血尿素氮;CALLY,C反应蛋白-白蛋白-淋巴细胞;CLR,C-反应蛋白与淋巴细胞比值;CCR,C-反应蛋白与血清钙比值。
表 4 各项因素及列线图模型预测AP患者预后不良的效能
Table 4. Efficacy of various factors and nomogram models in predicting poor prognosis in AP patients
指标 AUC SE P值 95%CI Cut-off 约登指数 灵敏度 特异度 BISAP评分 0.705 0.038 <0.001 0.631~0.779 3.500 0.280 0.407 0.873 APACHE Ⅱ评分 0.830 0.031 <0.001 0.768~0.891 10.500 0.524 0.833 0.691 血清淀粉酶 0.792 0.034 <0.001 0.724~0.859 316.300 0.443 0.630 0.813 血清脂肪酶 0.775 0.039 <0.001 0.699~0.852 471.100 0.523 0.667 0.856 CALLY指数 0.738 0.030 <0.001 0.680~0.797 4.405 0.430 0.615 0.815 CLR 0.765 0.039 <0.001 0.688~0.842 72.445 0.503 0.704 0.799 CCR 0.787 0.034 <0.001 0.719~0.854 19.200 0.423 0.630 0.793 列线图模型 0.977 0.007 <0.001 0.963~0.991 0.107 0.861 0.963 0.898 注:BISAP,严重程度床边指数;APACHE Ⅱ,急性生理学与慢性健康状况评价Ⅱ;CALLY,C反应蛋白-白蛋白-淋巴细胞;CLR,C-反应蛋白与淋巴细胞比值;CCR,C-反应蛋白与血清钙比值;AUC,受试者操作特征曲线下面积。
-
[1] WANG SP, ZHANG J, ZHANG K, et al. Predictive value of visceral adiposity index on the severity of hyperlipidemia-induced acute pancreatitis[J]. Chin J Integr Tradit West Med Intensive Crit Care, 2023, 30( 4): 453- 457. DOI: 10.3969/j.issn.1008-9691.2023.04.013.王思盼, 张珏, 张珂, 等. 内脏脂肪指数对高脂血症性急性胰腺炎患者病情严重程度的预测价值[J]. 中国中西医结合急救杂志, 2023, 30( 4): 453- 457. DOI: 10.3969/j.issn.1008-9691.2023.04.013. [2] FENG QZ, LU MM, SUN J, et al. Novel markers of systemic inflammation in prediction of the early severity of acute pancreatitis[J]. J Pract Med, 2024, 40( 14): 1963- 1968. DOI: 10.3969/j.issn.1006-5725.2024.14.011.冯其柱, 卢曼曼, 孙杰, 等. 新型全身性炎症指标对急性胰腺炎早期病情严重程度的预测价值[J]. 实用医学杂志, 2024, 40( 14): 1963- 1968. DOI: 10.3969/j.issn.1006-5725.2024.14.011. [3] KNOPH CS, COOK ME, NOVOVIC S, et al. No effect of methylnaltrexone on acute pancreatitis severity: A multicenter randomized controlled trial[J]. Am J Gastroenterol, 2024, 119( 11): 2307- 2316. DOI: 10.14309/ajg.0000000000002904. [4] SUN B, BAI R, SUI YH. Implementation and strategy of surgical rescue in the treatment of severe acute pancreatitis[J]. Chin J Dig Surg, 2024, 23( 5): 653- 657. DOI: 10.3760/cma.j.cn115610-20240301-00138.孙备, 白睿, 隋宇航. 重症急性胰腺炎外科救援的实施与策略[J]. 中华消化外科杂志, 2024, 23( 5): 653- 657. DOI: 10.3760/cma.j.cn115610-20240301-00138. [5] LIU Y, SHUAI JY, YANG ZY, et al. Diagnosis of acute pancreatitis severity and prognosis by pulmonary ultrasound scoring[J]. Chin J Exp Surg, 2023, 40( 7): 1397- 1400. DOI: 10.3760/cma.j.cn421213-20230607-01394.刘英, 帅佳颖, 杨治宇, 等. 肺超声评分鉴别急性胰腺炎病情危重程度及预后评估[J]. 中华实验外科杂志, 2023, 40( 7): 1397- 1400. DOI: 10.3760/cma.j.cn421213-20230607-01394. [6] MA XD, LIU ZN. Research progress in the value of neutrophil-to-lymphocyte ratio in the evaluation of disease severity of severe acute pancreatitis[J]. Chin J Pract Intern Med, 2023, 43( 6): 518- 521. DOI: 10.19538/j.nk2023060114.马晓迪, 刘振宁. 中性粒细胞/淋巴细胞比值对重症急性胰腺炎病情严重程度及预后评估价值的研究进展[J]. 中国实用内科杂志, 2023, 43( 6): 518- 521. DOI: 10.19538/j.nk2023060114. [7] GONG CJ, LIU L, LIU JJ, et al. Detection of systemic immune-inflammatory index combined with peripheral blood neutrophil-to-lymphocyte ratio and D-dimer-to-fibrinogen ratio for prognostic assessment in patients with acute pancreatitis[J]. Clin J Med Off, 2024, 52( 3): 324- 326, 330. DOI: 10.16680/j.1671-3826.2024.03.29.龚川江, 刘利, 刘佳佳, 等. 全身免疫炎症指数联合外周血中性粒细胞/淋巴细胞比值、D-二聚体/纤维蛋原比值检测对急性胰腺炎患者预后评估价值[J]. 临床军医杂志, 2024, 52( 3): 324- 326, 330. DOI: 10.16680/j.1671-3826.2024.03.29. [8] XU DD, XIAO AQ, YANG WS, et al. CT radiomics and clinical indicators combined model in early prediction the severity of acute pancreatitis[J]. Chin J Emerg Med, 2024, 33( 10): 1383- 1389. DOI: 10.3760/cma.j.issn.1671-0282.2024.10.007.徐丹丹, 肖奥齐, 杨维森, 等. CT影像组学-临床指标联合模型早期预测急性胰腺炎严重程度[J]. 中华急诊医学杂志, 2024, 33( 10): 1383- 1389. DOI: 10.3760/cma.j.issn.1671-0282.2024.10.007. [9] BULDUKOGLU OC. Potential future predictors of disease severity and persistent organ failure in acute pancreatitis[J]. J Clin Gastroenterol, 2024, 58( 6): 632- 633. DOI: 10.1097/MCG.0000000000002008. [10] XU HM, GUO CX, LI YC, et al. Predictive value of nutritional risk index, systemic immune inflammation index and triglyceride glucose index on the condition and prognosis of patients with acute pancreatitis[J]. J Xi’an Jiaotong Univ Med Sci, 2023, 44( 4): 577- 582. DOI: 10.7652/jdyxb202304013.许海梅, 郭春宣, 李永超, 等. 营养风险指数、全身免疫炎症指数和三酰甘油葡萄糖指数预测急性胰腺炎患者病情及预后的价值[J]. 西安交通大学学报(医学版), 2023, 44( 4): 577- 582. DOI: 10.7652/jdyxb202304013. [11] WANG YD, WANG MM, GUO CM, et al. Establishment and validation of an early prediction model for severity of acute pancreatitis[J]. J Cap Med Univ, 2023, 44( 2): 302- 310. DOI: 10.3969/j.issn.1006-7795.2023.02.018.王亚丹, 王苗苗, 郭春梅, 等. 急性胰腺炎严重程度早期预测模型的构建与验证[J]. 首都医科大学学报, 2023, 44( 2): 302- 310. DOI: 10.3969/j.issn.1006-7795.2023.02.018. [12] LU F, ZHANG Y, YU J, et al. Clinical value of BISAP score combined with CRP and NLR in evaluating the severity of acute pancreatitis[J]. Medicine, 2023, 102( 45): e35934. DOI: 10.1097/MD.0000000000035934. [13] YU YC, JIN Z, SUN L. Risk factors associated with pancreatitis severity and pregnancy outcomes in patients with acute pancreatitis in pregnancy[J]. J China Med Univ, 2023, 52( 1): 73- 76, 80. DOI: 10.12007/j.issn.0258-4646.2023.01.014.于彦超, 金镇, 孙磊. 妊娠合并急性胰腺炎患者胰腺炎严重程度的危险因素及其妊娠结局[J]. 中国医科大学学报, 2023, 52( 1): 73- 76, 80. DOI: 10.12007/j.issn.0258-4646.2023.01.014. [14] Pancreas Study Group, Chinese Society of Gastroenterology, Chinese Medical Association; Editorial Board of Chinese Journal of Pancreatology; Editorial Board of Chinese Journal of Digestion. Chinese guidelines for the management of acute pancreatitis( Shenyang, 2019)[J]. J Clin Hepatol, 2019, 35( 12): 2706- 2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013.中华医学会消化病学分会胰腺疾病学组,《中华胰腺病杂志》编委会,《中华消化杂志》编委会. 中国急性胰腺炎诊治指南(2019年,沈阳)[J]. 临床肝胆病杂志, 2019, 35( 12): 2706- 2711. DOI: 10.3969/j.issn.1001-5256.2019.12.013. [15] BANKS PA, BOLLEN TL, DERVENIS C, et al. Classification of acute pancreatitis: 2012: Revision of the Atlanta classification and definitions by international consensus[J]. Gut, 2013, 62( 1): 102- 111. DOI: 10.1136/gutjnl-2012-302779. [16] WANG YZ, YUN YL, XIE J, et al. Value of five scoring systems in predicting the severity of hyperlipidemic acute pancreatitis: A comparative analysis[J]. J Clin Hepatol, 2023, 39( 6): 1391- 1397. DOI: 10.3969/j.issn.1001-5256.2023.06.020.王鵷臻, 员雅玲, 谢娟, 等. 五种评分系统预测高甘油三酯血症性急性胰腺炎严重程度的比较[J]. 临床肝胆病杂志, 2023, 39( 6): 1391- 1397. DOI: 10.3969/j.issn.1001-5256.2023.06.020. [17] HOU SB, WANG SL, YOU YT, et al. New model for predicting the development of pancreatic pseudocyst secondary to acute pancreatitis[J]. Medicine, 2023, 102( 47): e36102. DOI: 10.1097/MD.0000000-000036102. [18] GOU YY, YAO L, CAO J. Changes in coagulation indices and D-dimer levels in hypertriglyceridemic acute pancreatitis and their value in predicting disease severity[J]. J Cent South Univ Med Sci, 2023, 48( 7): 1050- 1058. DOI: 10.11817/j.issn.1672-7347.2023.230155.苟园园, 姚隆, 曹洁. 高甘油三酯血症性急性胰腺炎凝血指标与D-二聚体水平变化及其预测疾病严重程度的价值[J]. 中南大学学报(医学版), 2023, 48( 7): 1050- 1058. DOI: 10.11817/j.issn.1672-7347.2023.230155. [19] YAKAH W, SHAH I, SKELTON-BADLANI D, et al. Circulating mitochondrial DNA as a diagnostic biomarker for predicting disease severity in patients with acute pancreatitis[J]. Gastroenterology, 2023, 164( 6): 1009- 1011. DOI: 10.1053/j.gastro.2023.01.013. [20] XU X, CHEN ZX. Correlation of the serum levels of adiponectin, omentin, and visfatin with the severity of acute pancreatitis[J]. J Clin Hepatol, 2024, 40( 9): 1848- 1852. DOI: 10.12449/JCH240920.许新, 陈章兴. 血清脂联素、网膜素及内脂素水平与急性胰腺炎严重程度的相关性分析[J]. 临床肝胆病杂志, 2024, 40( 9): 1848- 1852. DOI: 10.12449/JCH240920. [21] LUO PP, LIU Q, HUANG LW. Value of triglyceride glucose-body mass index in evaluating the severity of hyperlipidemic acute pancreatitis[J]. J Clin Hepatol, 2024, 40( 8): 1661- 1665. DOI: 10.12449/JCH240824.罗萍萍, 刘群, 黄丽雯. 甘油三酯葡萄糖体质量指数(TyG-BMI)对高脂血症性急性胰腺炎严重程度的预测价值[J]. 临床肝胆病杂志, 2024, 40( 8): 1661- 1665. DOI: 10.12449/JCH240824. [22] ANSEL-WALLOIS W, ASSAKO P, YZET T, et al. Acute pancreatitis and computed tomography: Interest of portal venous phase alone in the initial phase[J]. Acta Radiol, 2024, 65( 8): 889- 897. DOI: 10.1177/02841851241260874. [23] LI YY, DING YL, JING SS, et al. Effect of vitamin D binding protein gene polymorphism on susceptibility and prognosis of severe acute pancreatitis[J]. Chin Crit Care Med, 2023, 35( 10): 1058- 1062. DOI: 10.3760/cma.j.cn121430-20230307-00145.李永元, 丁元林, 井树森, 等. 维生素D结合蛋白基因多态性对重症急性胰腺炎易感性及预后的影响[J]. 中华危重病急救医学, 2023, 35( 10): 1058- 1062. DOI: 10.3760/cma.j.cn121430-20230307-00145. [24] XU LJ, LI FX, WU JH, et al. The current status of early nursing for emergency pancreatitis and analysis of factors influencing prognosis: A retrospective study[J]. Medicine, 2024, 103( 39): e39662. DOI: 10.1097/MD.0000000000039662. [25] WU C, XING YM, ZHOU T, et al. Expression level of serum miR-29a in elderly patients with acute pancreatitis and its predictive value for complicated acute kidney injury[J]. Chin J Gerontol, 2023, 43( 18): 4392- 4394. DOI: 10.3969/j.issn.1005-9202.2023.18.013.吴冲, 邢益门, 周婷, 等. 老年急性胰腺炎患者血清miR-29a表达水平及其对并发急性肾损伤的预测价值[J]. 中国老年学杂志, 2023, 43( 18): 4392- 4394. DOI: 10.3969/j.issn.1005-9202.2023.18.013. [26] VINGE-HOLMQUIST O, BENTH JŠ, ARNØ E, et al. Increased incidence and reduced mortality after first attack of acute pancreatitis over an 18-year period[J]. Scand J Gastroenterol, 2023, 58( 12): 1534- 1541. DOI: 10.1080/00365521.2023.2235452. [27] LI RJ, PENG Y, TANG XL, et al. Establishment of a modified BISAP scoring system and its clinical significance in the early diagnosis and prognostic evaluation of severe acute pancreatitis[J]. J Clin Hepatol, 2023, 39( 10): 2432- 2442. DOI: 10.3969/j.issn.1001-5256.2023.10.022.李蓉洁, 彭依, 唐小龙, 等. 改良BISAP评分系统的建立及其在重症急性胰腺炎早期诊断和预后评估中的意义[J]. 临床肝胆病杂志, 2023, 39( 10): 2432- 2442. DOI: 10.3969/j.issn.1001-5256.2023.10.022. [28] WENG Y, JIN L, CHU YX, et al. Comparison of prognostic value of different scoring systems in elderly patients with acute pancreatitis based on the newly revised Atlanta criteria[J]. Chin J Clin Pharmacol, 2024, 40( 16): 2329- 2333. DOI: 10.13699/j.cnki.1001-6821.2024.16.006.翁艳, 金鳞, 褚云香, 等. 不同评分系统对基于新修订Atlanta标准的老年急性胰腺炎患者预后预测价值的比较[J]. 中国临床药理学杂志, 2024, 40( 16): 2329- 2333. DOI: 10.13699/j.cnki.1001-6821.2024.16.006. [29] SONG HY, TAN QQ, YUAN Y, et al. Preoperative acute pancreatitis and hyperenzymemia are associated with poor prognosis in patients with nonfunctional pancreatic neuroendocrine tumors[J]. J Surg Oncol, 2023, 127( 7): 1135- 1142. DOI: 10.1002/jso.27227. [30] GAO JY, WANG CH, FU XY, et al. Clinical characteristics and prognosis of 227 children with acute pancreatitis[J]. Chin Crit Care Med, 2024, 36( 6): 630- 634. DOI: 10.3760/cma.j.cn121430-20240219-00146.高敬岩, 汪朝慧, 傅小云, 等. 227例儿童急性胰腺炎的临床特征和预后分析[J]. 中华危重病急救医学, 2024, 36( 6): 630- 634. DOI: 10.3760/cma.j.cn121430-20240219-00146. [31] YU Y, YUAN F, SONG PA, et al. Application of lipid apheresis in acute lipogenic pancreatitis[J]. Blood Purif, 2024, 53( 6): 493- 499. DOI: 10.1159/000536301. [32] HAN BH, YANG W, WANG H, et al. Construction and evaluation of a prognostic model for severe acute pancreatitis based on CT scores and inflammatory factors[J]. Chin Crit Care Med, 2023, 35( 1): 82- 87. DOI: 10.3760/cma.j.cn121430-20220411-00351.韩宝华, 杨文, 王慧, 等. 基于CT评分和炎症因子的重症急性胰腺炎预后模型构建及评价[J]. 中华危重病急救医学, 2023, 35( 1): 82- 87. DOI: 10.3760/cma.j.cn121430-20220411-00351. -



 PDF下载 ( 1456 KB)
PDF下载 ( 1456 KB)

 下载:
下载: