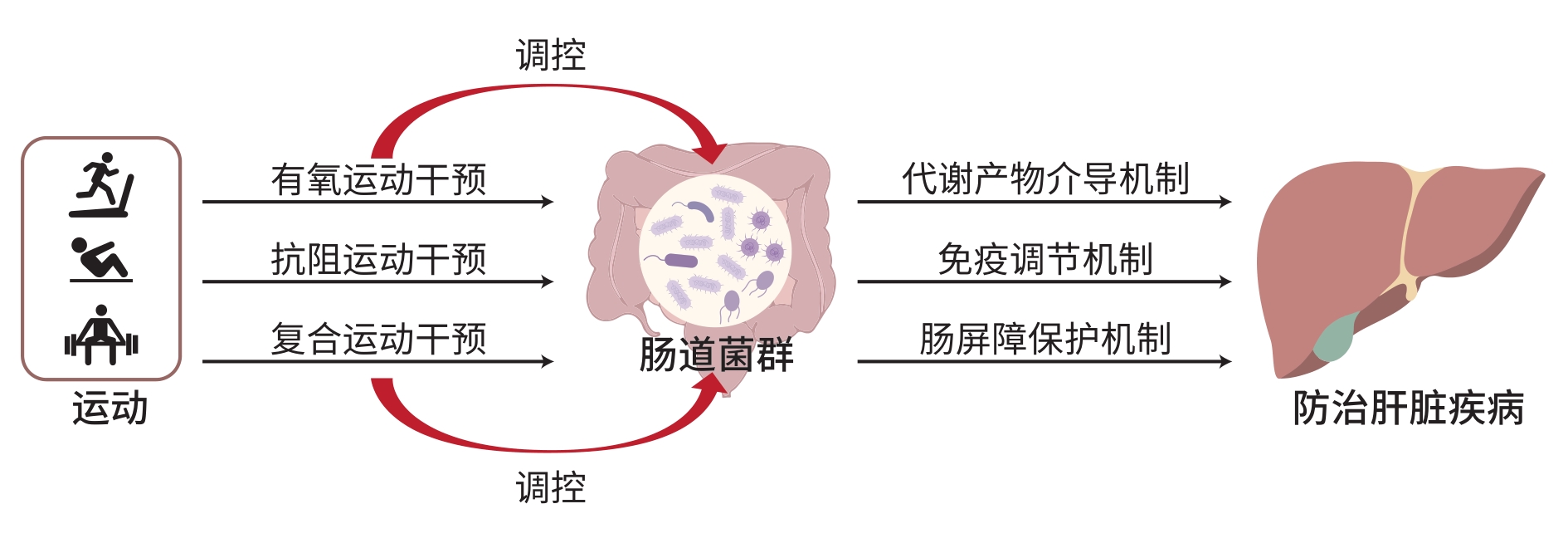
运动调控肠道菌群在肝脏疾病防治中的作用
DOI: 10.12449/JCH250834
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:徐珍负责收集与分析资料,撰写文章;廖粤生负责设计文章架构,撰写与修改文章;冯晓露负责指导撰写文章。
The role of exercise in the prevention and treatment of liver diseases by regulating intestinal flora
-
摘要: 肝脏疾病具有发病机制复杂、病情发展多样以及治疗难度较大等特点,其发病率在全球范围内呈逐年上升趋势,给家庭和社会带来了沉重的医疗负担。运动作为一种非药物性、安全性高、可操作性强的干预手段,近年来被发现与肠道菌群之间存在着紧密的联系,且由运动引发的肠道菌群良性改变还可能对肝功能产生积极影响。本文对近年运动调控肠道菌群防治肝脏疾病的前沿研究成果加以总结,以期为防治肝脏疾病提供理论参考。Abstract: Liver diseases are characterized by complex pathogeneses, diverse patterns of disease progression, and difficulties in treatment, and their incidence rates are increasing year by year globally, bringing a heavy medical burden to families and society. Recent studies have shown that as a non-pharmacological intervention measure with high safety and strong operability, exercise is closely associated with intestinal flora, and the benign changes in intestinal flora triggered by exercise may also have a positive effect on liver function. This article summarizes the recent research findings of exercise in the prevention and treatment of liver diseases by regulating intestinal flora, in order to provide a theoretical reference for the prevention and treatment of liver diseases.
-
Key words:
- Exercise /
- Gastrointestinal Microbiome /
- Liver Disease
-
[1] WEN YK, MA LC, JU C. Recent insights into the pathogenesis and therapeutic targets of chronic liver diseases[J]. eGastroenterology, 2023, 1( 2): e100020. DOI: 10.1136/egastro-2023-100020. [2] UNAGOLLA JM, DAS S, FLANAGAN R, et al. Targeting chronic liver diseases: Molecular markers, drug delivery strategies and future perspectives[J]. Int J Pharm, 2024, 660: 124381. DOI: 10.1016/j.ijpharm.2024.124381. [3] WANG R, TANG RQ, LI B, et al. Gut microbiome, liver immunology, and liver diseases[J]. Cell Mol Immunol, 2021, 18( 1): 4- 17. DOI: 10.1038/s41423-020-00592-6. [4] ZHANG LL, ZI LL, KUANG TR, et al. Investigating causal associations among gut microbiota, metabolites, and liver diseases: A Mendelian randomization study[J]. Front Endocrinol(Lausanne), 2023, 14: 1159148. DOI: 10.3389/fendo.2023.1159148. [5] TILG H, CANI PD, MAYER EA. Gut microbiome and liver diseases[J]. Gut, 2016, 65( 12): 2035- 2044. DOI: 10.1136/gutjnl-2016-312729. [6] CLAUSS M, GÉRARD P, MOSCA A, et al. Interplay between exercise and gut microbiome in the context of human health and performance[J]. Front Nutr, 2021, 8: 637010. DOI: 10.3389/fnut.2021.637010. [7] MAILING LJ, ALLEN JM, BUFORD TW, et al. Exercise and the gut microbiome: A review of the evidence, potential mechanisms, and implications for human health[J]. Exerc Sport Sci Rev, 2019, 47( 2): 75- 85. DOI: 10.1249/JES.0000000000000183. [8] LIU SY, YANG XL. Intestinal flora plays a role in the progression of hepatitis-cirrhosis-liver cancer[J]. Front Cell Infect Microbiol, 2023, 13: 1140126. DOI: 10.3389/fcimb.2023.1140126. [9] HSU CL, SCHNABL B. The gut-liver axis and gut microbiota in health and liver disease[J]. Nat Rev Microbiol, 2023, 21( 11): 719- 733. DOI: 10.1038/s41579-023-00904-3. [10] TILG H, ADOLPH TE, TRAUNER M. Gut-liver axis: Pathophysiological concepts and clinical implications[J]. Cell Metab, 2022, 34( 11): 1700- 1718. DOI: 10.1016/j.cmet.2022.09.017. [11] ALBHAISI SAM, BAJAJ JS, SANYAL AJ. Role of gut microbiota in liver disease[J]. Am J Physiol Gastrointest Liver Physiol, 2020, 318( 1): G84- G98. DOI: 10.1152/ajpgi.00118.2019. [12] WANG DD, SONG J, ZHANG XL. Research advances in the role of gut microbiota in liver diseases[J]. J Clin Hepatol, 2019, 35( 9): 2120- 2123. DOI: 10.3969/j.issn.1001-5256.2019.09.053.王丹丹, 宋佳, 张晓岚. 肠道菌群在肝脏疾病中的作用[J]. 临床肝胆病杂志, 2019, 35( 9): 2120- 2123. DOI: 10.3969/j.issn.1001-5256.2019.09.053. [13] WEI QQ, XIANG J. Research progress on the potential role of exercise intervention in Parkinson’s disease based on in-testinal flora[J]. Prog Physiol Sci, 2024, 55( 4): 353- 360. DOI: 10.20059/j.cnki.pps.2024.03.1166.韦泉清, 项洁. 基于肠道菌群的运动干预帕金森病可能机制的研究进展[J]. 生理科学进展, 2024, 55( 4): 353- 360. DOI: 10.20059/j.cnki.pps.2024.03.1166. [14] DUNN W, SHAH VH. Pathogenesis of alcoholic liver disease[J]. Clin Liver Dis, 2016, 20( 3): 445- 456. DOI: 10.1016/j.cld.2016.02.004. [15] YAN CY, HU WT, TU JQ, et al. Pathogenic mechanisms and regulatory factors involved in alcoholic liver disease[J]. J Transl Med, 2023, 21( 1): 300. DOI: 10.1186/s12967-023-04166-8. [16] KAKIYAMA G, PANDAK WM, GILLEVET PM, et al. Modulation of the fecal bile acid profile by gut microbiota in cirrhosis[J]. J Hepatol, 2013, 58( 5): 949- 955. DOI: 10.1016/j.jhep.2013.01.003. [17] JIANG CT, XIE C, LI F, et al. Intestinal farnesoid X receptor signaling promotes nonalcoholic fatty liver disease[J]. J Clin Invest, 2015, 125( 1): 386- 402. DOI: 10.1172/JCI76738. [18] BOURSIER J, MUELLER O, BARRET M, et al. The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota[J]. Hepatology, 2016, 63( 3): 764- 775. DOI: 10.1002/hep.28356. [19] LURIE Y, WEBB M, CYTTER-KUINT R, et al. Non-invasive diagnosis of liver fibrosis and cirrhosis[J]. World J Gastroenterol, 2015, 21( 41): 11567- 11583. DOI: 10.3748/wjg.v21.i41.11567. [20] PAROLA M, PINZANI M. Liver fibrosis: Pathophysiology, pathogenetic targets and clinical issues[J]. Mol Aspects Med, 2019, 65: 37- 55. DOI: 10.1016/j.mam.2018.09.002. [21] LEE NY, SUK KT. The role of the gut microbiome in liver cirrhosis treatment[J]. Int J Mol Sci, 2020, 22( 1): 199. DOI: 10.3390/ijms22010199. [22] LAPIDOT Y, AMIR A, NOSENKO R, et al. Alterations in the gut microbiome in the progression of cirrhosis to hepatocellular carcinoma[J]. mSystems, 2020, 5( 3): e00153-20. DOI: 10.1128/mSystems.00153-20. [23] OIKONOMOU T, PAPATHEODORIDIS GV, SAMARKOS M, et al. Clinical impact of microbiome in patients with decompensated cirrhosis[J]. World J Gastroenterol, 2018, 24( 34): 3813- 3820. DOI: 10.3748/wjg.v24.i34.3813. [24] WANG RH, CAI YY, LU WC, et al. Exercise effect on the gut microbiota in young adolescents with subthreshold depression: A randomized psychoeducation-controlled Trial[J]. Psychiatry Res, 2023, 319: 115005. DOI: 10.1016/j.psychres.2022.115005. [25] ZHU YP, ZHU J, SONG G. The impact of aerobic exercise training on cognitive function and gut microbiota in methamphetamine-dependent individuals in the community[J]. Physiol Behav, 2023, 270: 114302. DOI: 10.1016/j.physbeh.2023.114302. [26] CULLEN JMA, SHAHZAD S, KANALEY JA, et al. The effects of 6 wk of resistance training on the gut microbiome and cardiometabolic health in young adults with overweight and obesity[J]. J Appl Physiol(1985), 2024, 136( 2): 349- 361. DOI: 10.1152/japplphysiol.00350.2023. [27] QUIROGA R, NISTAL E, ESTÉBANEZ B, et al. Exercise training modulates the gut microbiota profile and impairs inflammatory signaling pathways in obese children[J]. Exp Mol Med, 2020, 52( 7): 1048- 1061. DOI: 10.1038/s12276-020-0459-0. [28] MOTIANI KK, CARMEN COLLADO M, ESKELINEN JJ, et al. Exercise training modulates gut microbiota profile and improves endotoxemia[J]. Med Sci Sports Exerc, 2020, 52( 1): 94- 104. DOI: 10.1249/MSS.0000000000002112. [29] GALLÈ F, VALERIANI F, CATTARUZZA MS, et al. Mediterranean diet, physical activity and gut microbiome composition: A cross-sectional study among healthy young Italian adults[J]. Nutrients, 2020, 12( 7): 2164. DOI: 10.3390/nu12072164. [30] HAMPTON-MARCELL JT, ESHOO TW, COOK MD, et al. Comparative analysis of gut microbiota following changes in training volume among swimmers[J]. Int J Sports Med, 2020, 41( 5): 292- 299. DOI: 10.1055/a-1079-5450. [31] LIANG R, ZHANG S, PENG XJ, et al. Characteristics of the gut microbiota in professional martial arts athletes: A comparison between different competition levels[J]. PLoS One, 2019, 14( 12): e0226240. DOI: 10.1371/journal.pone.0226240. [32] BYCURA D, SANTOS AC, SHIFFER A, et al. Impact of different exercise modalities on the human gut microbiome[J]. Sports(Basel), 2021, 9( 2): 14. DOI: 10.3390/sports9020014. [33] O'DONOVAN CM, MADIGAN SM, GARCIA-PEREZ I, et al. Distinct microbiome composition and metabolome exists across subgroups of elite Irish athletes[J]. J Sci Med Sport, 2020, 23( 1): 63- 68. DOI: 10.1016/j.jsams.2019.08.290. [34] VOIGT RM, FORSYTH CB, GREEN SJ, et al. Circadian rhythm and the gut microbiome[J]. Int Rev Neurobiol, 2016, 131: 193- 205. DOI: 10.1016/bs.irn.2016.07.002. [35] LIANG X, BUSHMAN FD, FITZGERALD GA. Rhythmicity of the intestinal microbiota is regulated by gender and the host circadian clock[J]. Proc Natl Acad Sci USA, 2015, 112( 33): 10479- 10484. DOI: 10.1073/pnas.1501305112. [36] GABRIEL BM, ZIERATH JR. Circadian rhythms and exercise—re-setting the clock in metabolic disease[J]. Nat Rev Endocrinol, 2019, 15( 4): 197- 206. DOI: 10.1038/s41574-018-0150-x. [37] ERLANDSON KM, LIU J, JOHNSON R, et al. An exercise intervention alters stool microbiota and metabolites among older, sedentary adults[J]. Ther Adv Infect Dis, 2021, 8: 20499361211027067. DOI: 10.1177/20499361211027067. [38] SHENG TJ, YAN SM, LAN WR, et al. Research progress on the effect of intestinal microorganisms on inflammatory bowel disease[J]. Clin J Med Offic, 2023, 51( 9): 904- 907. DOI: 10.16680/j.1671-3826.2023.09.06.盛天骄, 闫思蒙, 兰威儒, 等. 肠道微生物对炎症性肠病影响研究进展[J]. 临床军医杂志, 2023, 51( 9): 904- 907. DOI: 10.16680/j.1671-3826.2023.09.06. [39] YO S, MATSUMOTO H, GU TT, et al. Exercise affects mucosa-associated microbiota and colonic tumor formation induced by azoxymethane in high-fat-diet-induced obese mice[J]. Microorganisms, 2024, 12( 5): 957. DOI: 10.3390/microorganisms12050957. [40] LIN DH, JIANG XX, ZHAO Y, et al. Komagataeibacter hansenii CGMCC 3917 alleviates alcohol-induced liver injury by regulating fatty acid metabolism and intestinal microbiota diversity in mice[J]. Food Funct, 2020, 11( 5): 4591- 4604. DOI: 10.1039/c9fo02040c. [41] BLAAK EE, CANFORA EE, THEIS S, et al. Short chain fatty acids in human gut and metabolic health[J]. Benef Microbes, 2020, 11( 5): 411- 455. DOI: 10.3920/BM2020.0057. [42] DENG MJ, QU F, CHEN L, et al. SCFAs alleviated steatosis and inflammation in mice with NASH induced by MCD[J]. J Endocrinol, 2020, 245( 3): 425- 437. DOI: 10.1530/JOE-20-0018. [43] YOU HM, TAN Y, YU DW, et al. The therapeutic effect of SCFA-mediated regulation of the intestinal environment on obesity[J]. Front Nutr, 2022, 9: 886902. DOI: 10.3389/fnut.2022.886902. [44] WANG YJ, PU ZJ, ZHANG YR, et al. Exercise training has a protective effect in 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine mice model with improved neural and intestinal pathology and modified intestinal flora[J]. Behav Brain Res, 2023, 439: 114240. DOI: 10.1016/j.bbr.2022.114240. [45] SMITH BK, MARCINKO K, DESJARDINS EM, et al. Treatment of nonalcoholic fatty liver disease: Role of AMPK[J]. Am J Physiol Endocrinol Metab, 2016, 311( 4): E730- E740. DOI: 10.1152/ajpendo.00225.2016. [46] WANG JJ, ZHU NN, SU XM, et al. Gut-microbiota-derived metabolites maintain gut and systemic immune homeostasis[J]. Cells, 2023, 12( 5): 793. DOI: 10.3390/cells12050793. [47] CODELLA R, LUZI L, TERRUZZI I. Exercise has the guts: How physical activity may positively modulate gut microbiota in chronic and immune-based diseases[J]. Dig Liver Dis, 2018, 50( 4): 331- 341. DOI: 10.1016/j.dld.2017.11.016. [48] COOK MD, ALLEN JM, PENCE BD, et al. Exercise and gut immune function: Evidence of alterations in colon immune cell homeostasis and microbiome characteristics with exercise training[J]. Immunol Cell Biol, 2016, 94( 2): 158- 163. DOI: 10.1038/icb.2015.108. [49] SONG MY, CHAN AT. The potential role of exercise and nutrition in harnessing the immune system to improve colorectal cancer survival[J]. Gastroenterology, 2018, 155( 3): 596- 600. DOI: 10.1053/j.gastro.2018.07.038. [50] GONZALEZ-GIL AM, ELIZONDO-MONTEMAYOR L. The role of exercise in the interplay between myokines, hepatokines, osteokines, adipokines, and modulation of inflammation for energy substrate redistribution and fat mass loss: A review[J]. Nutrients, 2020, 12( 6): 1899. DOI: 10.3390/nu12061899. [51] DI TOMMASO N, GASBARRINI A, PONZIANI FR. Intestinal barrier in human health and disease[J]. Int J Environ Res Public Health, 2021, 18( 23): 12836. DOI: 10.3390/ijerph182312836. [52] GHOSH S, WHITLEY CS, HARIBABU B, et al. Regulation of intestinal barrier function by microbial metabolites[J]. Cell Mol Gastroenterol Hepatol, 2021, 11( 5): 1463- 1482. DOI: 10.1016/j.jcmgh.2021.02.007. [53] PASINI E, CORSETTI G, ASSANELLI D, et al. Effects of chronic exercise on gut microbiota and intestinal barrier in human with type 2 diabetes[J]. Minerva Med, 2019, 110( 1): 3- 11. DOI: 10.23736/S0026-4806.18.05589-1. [54] FREITAS AL, SILVA MB, SILVA CS, et al. Alanyl-glutamine protects the intestinal barrier function in trained rats against the impact of acute exhaustive exercise[J]. Braz J Med Biol Res, 2020, 53( 5): e9211. DOI: 10.1590/1414-431X20209211. [55] YUAN SL, YANG JL, JIAN Y, et al. Treadmill exercise modulates intestinal microbes and suppresses LPS displacement to alleviate neuroinflammation in the brains of APP/PS1 mice[J]. Nutrients, 2022, 14( 19): 4134. DOI: 10.3390/nu14194134. -



 PDF下载 ( 953 KB)
PDF下载 ( 953 KB)

 下载:
下载:


