酒精性肝病增加脓毒症易感性机制的研究进展
DOI: 10.12449/JCH250829
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:郭焱负责课题设计,指导撰写文章并最后定稿;刘航负责资料收集分析,撰写论文。
Research advances in the mechanisms of increased susceptibility to sepsis in alcoholic liver disease
-
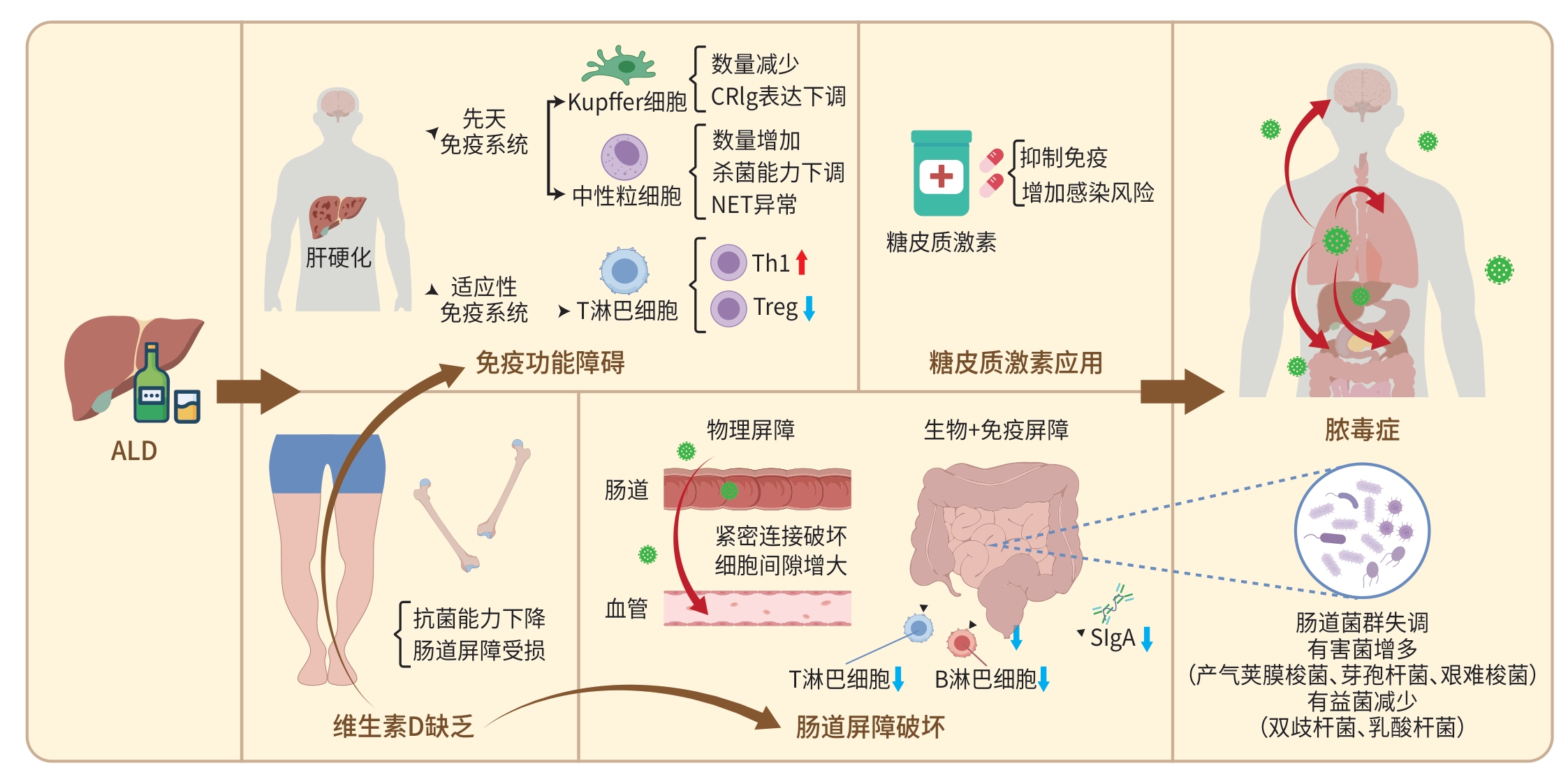
摘要: 脓毒症是由宿主对感染的反应失调导致危及生命的器官功能障碍,目前尚缺乏有效的治疗方法。酒精性肝病(ALD)是西方国家酒精导致死亡的最重要原因。脓毒症是ALD最常见的并发症和死亡原因之一,本文对ALD增加脓毒症易感性机制的研究进展进行综述,旨在为ALD致脓毒症患者的预防和治疗提供参考。Abstract: Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection, and currently there is still a lack of effective therapies. Alcoholic liver disease (ALD) is the most important cause of death caused by alcohol in Western countries, and sepsis is one of the most common complications and causes of death in ALD. This article reviews the research advances in the mechanism by which ALD increases the susceptibility to sepsis, in order to provide a reference for the prevention and treatment of sepsis in ALD patients.
-
Key words:
- Sepsis /
- Alcoholic Liver Disease /
- Immune System /
- Gastrointestinal Microbiome
-
[1] SINGER M, DEUTSCHMAN CS, SEYMOUR CW, et al. The third international consensus definitions for sepsis and septic shock(sepsis-3)[J]. JAMA, 2016, 315( 8): 801- 810. DOI: 10.1001/jama.2016.0287. [2] DONG R, LIU W, WENG L, et al. Temporal trends of sepsis-related mortality in China, 2006-2020: A population-based study[J]. Ann Intensive Care, 2023, 13( 1): 71. DOI: 10.1186/s13613-023-01166-1. [3] GUSTOT T, FERNANDEZ J, SZABO G, et al. Sepsis in alcohol-related liver disease[J]. J Hepatol, 2017, 67( 5): 1031- 1050. DOI: 10.1016/j.jhep.2017.06.013. [4] JOPHLIN LL, SINGAL AK, BATALLER R, et al. ACG clinical guideline: Alcohol-associated liver disease[J]. Am J Gastroenterol, 2024, 119( 1): 30- 54. DOI: 10.14309/ajg.0000000000002572. [5] GUSTOT T, JALAN R. Acute-on-chronic liver failure in patients with alcohol-related liver disease[J]. J Hepatol, 2019, 70( 2): 319- 327. DOI: 10.1016/j.jhep.2018.12.008. [6] World Health Organization. Global status report on alcohol and health 2018[G]. World Health Organization, 2018. [7] NAGHAVI M, ABAJOBIR AA, ABBAFATI C, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: A systematic analysis for the Global Burden of Disease Study 2016[J]. Lancet, 2017, 390( 10100): 1151- 1210. DOI: 10.1016/S0140-6736(17)32152-9. [8] WANG YK, WANG MQ, LIU CR, et al. Global burden of liver cirrhosis 1990-2019 and 20 years forecast: Results from the global burden of disease study 2019[J]. Ann Med, 2024, 56( 1): 2328521. DOI: 10.1080/07853890.2024.2328521. [9] BONNEL AR, BUNCHORNTAVAKUL C, RAJENDER REDDY K. Immune dysfunction and infections in patients with cirrhosis[J]. Clin Gastroenterol Hepatol, 2011, 9( 9): 727- 738. DOI: 10.1016/j.cgh.2011.02.031. [10] NOOR MT, MANORIA P. Immune dysfunction in cirrhosis[J]. J Clin Transl Hepatol, 2017, 5( 1): 50- 58. DOI: 10.14218/JCTH.2016.00056. [11] ALBILLOS A, MARTIN-MATEOS R, van der MERWE S, et al. Cirrhosis-associated immune dysfunction[J]. Nat Rev Gastroenterol Hepatol, 2022, 19( 2): 112- 134. DOI: 10.1038/s41575-021-00520-7. [12] SZABO G, PETRASEK J, BALA SS. Innate immunity and alcoholic liver disease[J]. Dig Dis, 2012, 30( Suppl 1): 55- 60. DOI: 10.1159/000341126. [13] LI S, TAN HY, WANG N, et al. Recent insights into the role of immune cells in alcoholic liver disease[J]. Front Immunol, 2019, 10: 1328. DOI: 10.3389/fimmu.2019.01328. [14] NAGY LE. The role of innate immunity in alcoholic liver disease[J]. Alcohol Res, 2015, 37( 2): 237- 250. [15] GAO B, AHMAD MF, NAGY LE, et al. Inflammatory pathways in alcoholic steatohepatitis[J]. J Hepatol, 2019, 70( 2): 249- 259. DOI: 10.1016/j.jhep.2018.10.023. [16] van LOOKEREN CAMPAGNE M, VERSCHOOR A. Pathogen clearance and immune adherence“revisited”: Immuno-regulatory roles for CRIg[J]. Semin Immunol, 2018, 37: 4- 11. DOI: 10.1016/j.smim.2018.02.007. [17] ZENG ZT, SUREWAARD BGJ, WONG CHY, et al. CRIg functions as a macrophage pattern recognition receptor to directly bind and capture blood-borne gram-positive bacteria[J]. Cell Host Microbe, 2016, 20( 1): 99- 106. DOI: 10.1016/j.chom.2016.06.002. [18] DUAN Y, CHU HK, BRANDL K, et al. CRIg on liver macrophages clears pathobionts and protects against alcoholic liver disease[J]. Nat Commun, 2021, 12( 1): 7172. DOI: 10.1038/s41467-021-27385-3. [19] JENNE CN, KUBES P. Immune surveillance by the liver[J]. Nat Immunol, 2013, 14( 10): 996- 1006. DOI: 10.1038/ni.2691. [20] PEISELER M, DAVID BA, ZINDEL J, et al. Kupffer cell-like syncytia replenish resident macrophage function in the fibrotic liver[J]. Science, 2023, 381( 6662): eabq5202. DOI: 10.1126/science.abq5202. [21] KHAN RS, LALOR PF, THURSZ M, et al. The role of neutrophils in alcohol-related hepatitis[J]. J Hepatol, 2023, 79( 4): 1037- 1048. DOI: 10.1016/j.jhep.2023.05.017. [22] HERRO R, LEIGHTON GRIMES H. The diverse roles of neutrophils from protection to pathogenesis[J]. Nat Immunol, 2024, 25( 12): 2209- 2219. DOI: 10.1038/s41590-024-02006-5. [23] PAPAYANNOPOULOS V. Neutrophil extracellular traps in immunity and disease[J]. Nat Rev Immunol, 2018, 18( 2): 134- 147. DOI: 10.1038/nri.2017.105. [24] MOOKERJEE RP, STADLBAUER V, LIDDER S, et al. Neutrophil dysfunction in alcoholic hepatitis superimposed on cirrhosis is reversible and predicts the outcome[J]. Hepatology, 2007, 46( 3): 831- 840. DOI: 10.1002/hep.21737. [25] BUKONG TN, CHO Y, IRACHETA-VELLVE A, et al. Abnormal neutrophil traps and impaired efferocytosis contribute to liver injury and sepsis severity after binge alcohol use[J]. J Hepatol, 2018, 69( 5): 1145- 1154. DOI: 10.1016/j.jhep.2018.07.005. [26] CHO Y, BUKONG TN, TORNAI D, et al. Neutrophil extracellular traps contribute to liver damage and increase defective low-density neutrophils in alcohol-associated hepatitis[J]. J Hepatol, 2023, 78( 1): 28- 44. DOI: 10.1016/j.jhep.2022.08.029. [27] McTERNAN PM, LEVITT DE, WELSH DA, et al. Alcohol impairs immunometabolism and promotes Naïve T cell differentiation to pro-inflammatory Th1 CD4+ T cells[J]. Front Immunol, 2022, 13: 839390. DOI: 10.3389/fimmu.2022.839390. [28] ZULUAGA P, ZURERA-EGEA C, FUSTER D, et al. Changes in CD4+ T cells subsets in patients with alcohol-related cirrhosis[J]. Clin Exp Med, 2025, 25( 1): 31. DOI: 10.1007/s10238-024-01548-0. [29] WANG R, TANG RQ, LI B, et al. Gut microbiome, liver immunology, and liver diseases[J]. Cell Mol Immunol, 2021, 18( 1): 4- 17. DOI: 10.1038/s41423-020-00592-6. [30] SOSNOWSKI K, PRZYBYŁKOWSKI A. Ethanol-induced changes to the gut microbiome compromise the intestinal homeostasis: A review[J]. Gut Microbes, 2024, 16( 1): 2393272. DOI: 10.1080/19490976.2024.2393272. [31] DI VINCENZO F, DEL GAUDIO A, PETITO V, et al. Gut microbiota, intestinal permeability, and systemic inflammation: A narrative review[J]. Intern Emerg Med, 2024, 19( 2): 275- 293. DOI: 10.1007/s11739-023-03374-w. [32] TULKENS J, VERGAUWEN G, van DEUN J, et al. Increased levels of systemic LPS-positive bacterial extracellular vesicles in patients with intestinal barrier dysfunction[J]. Gut, 2020, 69( 1): 191- 193. DOI: 10.1136/gutjnl-2018-317726. [33] PATEL S, BEHARA R, SWANSON GR, et al. Alcohol and the intestine[J]. Biomolecules, 2015, 5( 4): 2573- 2588. DOI: 10.3390/biom5042573. [34] MEENA AS, SHUKLA PK, BELL B, et al. TRPV6 channel mediates alcohol-induced gut barrier dysfunction and systemic response[J]. Cell Rep, 2022, 39( 11): 110937. DOI: 10.1016/j.celrep.2022.110937. [35] RUNGRATANAWANICH W, LIN YH, WANG X, et al. ALDH2 deficiency increases susceptibility to binge alcohol-induced gut leakiness, endotoxemia, and acute liver injury in mice through the gut-liver axis[J]. Redox Biol, 2023, 59: 102577. DOI: 10.1016/j.redox.2022.102577. [36] MACCIONI L, LECLERCQ IA, SCHNABL B, et al. Host factors in dysregulation of the gut barrier function during alcohol-associated liver disease[J]. Int J Mol Sci, 2021, 22( 23): 12687. DOI: 10.3390/ijms222312687. [37] INAMINE T, SCHNABL B. Immunoglobulin A and liver diseases[J]. J Gastroenterol, 2018, 53( 6): 691- 700. DOI: 10.1007/s00535-017-1400-8. [38] HENDRIKX T, LANG S, RAJCIC D, et al. Hepatic pIgR-mediated secretion of IgA limits bacterial translocation and prevents ethanol-induced liver disease in mice[J]. Gut, 2023, 72( 10): 1959- 1970. DOI: 10.1136/gutjnl-2022-328265. [39] MACCIONI L, GAO B, LECLERCQ S, et al. Intestinal permeability, microbial translocation, changes in duodenal and fecal microbiota, and their associations with alcoholic liver disease progression in humans[J]. Gut Microbes, 2020, 12( 1): 1782157. DOI: 10.1080/19490976.2020.1782157. [40] MACCIONI L, LORIOT A, DEWULF J, et al. Duodenal CD8+ T resident memory cell apoptosis contributes to gut barrier dysfunction and microbial translocation in early alcohol-associated liver disease in humans[J]. Aliment Pharmacol Ther, 2022, 56( 6): 1055- 1070. DOI: 10.1111/apt.17177. [41] DUKIĆ M, RADONJIĆ T, JOVANOVIĆ I, et al. Alcohol, inflammation, and microbiota in alcoholic liver disease[J]. Int J Mol Sci, 2023, 24( 4): 3735. DOI: 10.3390/ijms24043735. [42] HSU CL, SCHNABL B. The gut-liver axis and gut microbiota in health and liver disease[J]. Nat Rev Microbiol, 2023, 21( 11): 719- 733. DOI: 10.1038/s41579-023-00904-3. [43] ADRIENNE WEISS G, HENNET T. Mechanisms and consequences of intestinal dysbiosis[J]. Cell Mol Life Sci, 2017, 74( 16): 2959- 2977. DOI: 10.1007/s00018-017-2509-x. [44] BLUEMEL S, WANG LR, KUELBS C, et al. Intestinal and hepatic microbiota changes associated with chronic ethanol administration in mice[J]. Gut Microbes, 2020, 11( 3): 265- 275. DOI: 10.1080/19490976.2019.1595300. [45] PHILIPS CA, AHAMED R, RAJESH S, et al. Long-term outcomes of stool transplant in alcohol-associated hepatitis-analysis of clinical outcomes, relapse, gut microbiota and comparisons with standard care[J]. J Clin Exp Hepatol, 2022, 12( 4): 1124- 1132. DOI: 10.1016/j.jceh.2022.01.001. [46] SHIBAMOTO A, KAJI K, NISHIMURA N, et al. Vitamin D deficiency exacerbates alcohol-related liver injury via gut barrier disruption and hepatic overload of endotoxin[J]. J Nutr Biochem, 2023, 122: 109450. DOI: 10.1016/j.jnutbio.2023.109450. [47] DELRUE C, SPEECKAERT R, DELANGHE JR, et al. Vitamin D deficiency: An underestimated factor in sepsis?[J]. Int J Mol Sci, 2023, 24( 3): 2924. DOI: 10.3390/ijms24032924. [48] KHAN MA, DAR HA, BABA MA, et al. Impact of vitamin D status in chronic liver disease[J]. J Clin Exp Hepatol, 2019, 9( 5): 574- 580. DOI: 10.1016/j.jceh.2019.03.001. [49] WANG HH, GONG WY, GAO JX, et al. Effects of vitamin D deficiency on chronic alcoholic liver injury[J]. Free Radic Biol Med, 2024, 224: 220- 231. DOI: 10.1016/j.freeradbiomed.2024.08.037. [50] PAREKH D, PATEL JM, SCOTT A, et al. Vitamin D deficiency in human and murine sepsis[J]. Crit Care Med, 2017, 45( 2): 282- 289. DOI: 10.1097/CCM.0000000000002095. [51] MATHURIN P, O’GRADY J, CARITHERS RL, et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: Meta-analysis of individual patient data[J]. Gut, 2011, 60( 2): 255- 260. DOI: 10.1136/gut.2010.224097. [52] VERGIS N, ATKINSON SR, KNAPP S, et al. In patients with severe alcoholic hepatitis, prednisolone increases susceptibility to infection and infection-related mortality, and is associated with high circulating levels of bacterial DNA[J]. Gastroenterology, 2017, 152( 5): 1068- 1077. e 4. DOI: 10.1053/j.gastro.2016.12.019. [53] THURSZ MR, RICHARDSON P, ALLISON M, et al. Prednisolone or pentoxifylline for alcoholic hepatitis[J]. N Engl J Med, 2015, 372( 17): 1619- 1628. DOI: 10.1056/NEJMoa1412278. -



 PDF下载 ( 1146 KB)
PDF下载 ( 1146 KB)

 下载:
下载:


