PINK1/Parkin信号通路介导的线粒体自噬在代谢相关脂肪性肝病中的作用及靶向治疗研究进展
DOI: 10.12449/JCH250828
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:朱胜金负责撰写论文;朱小灯、李开楊负责设计论文框架及指导撰写文章并最后定稿;杨梅、吴娴负责论文修改。
Role of mitophagy induced by the PTEN-induced kinase 1/Parkin signaling pathway in metabolic associated fatty liver disease and related advances in targeted therapies
-
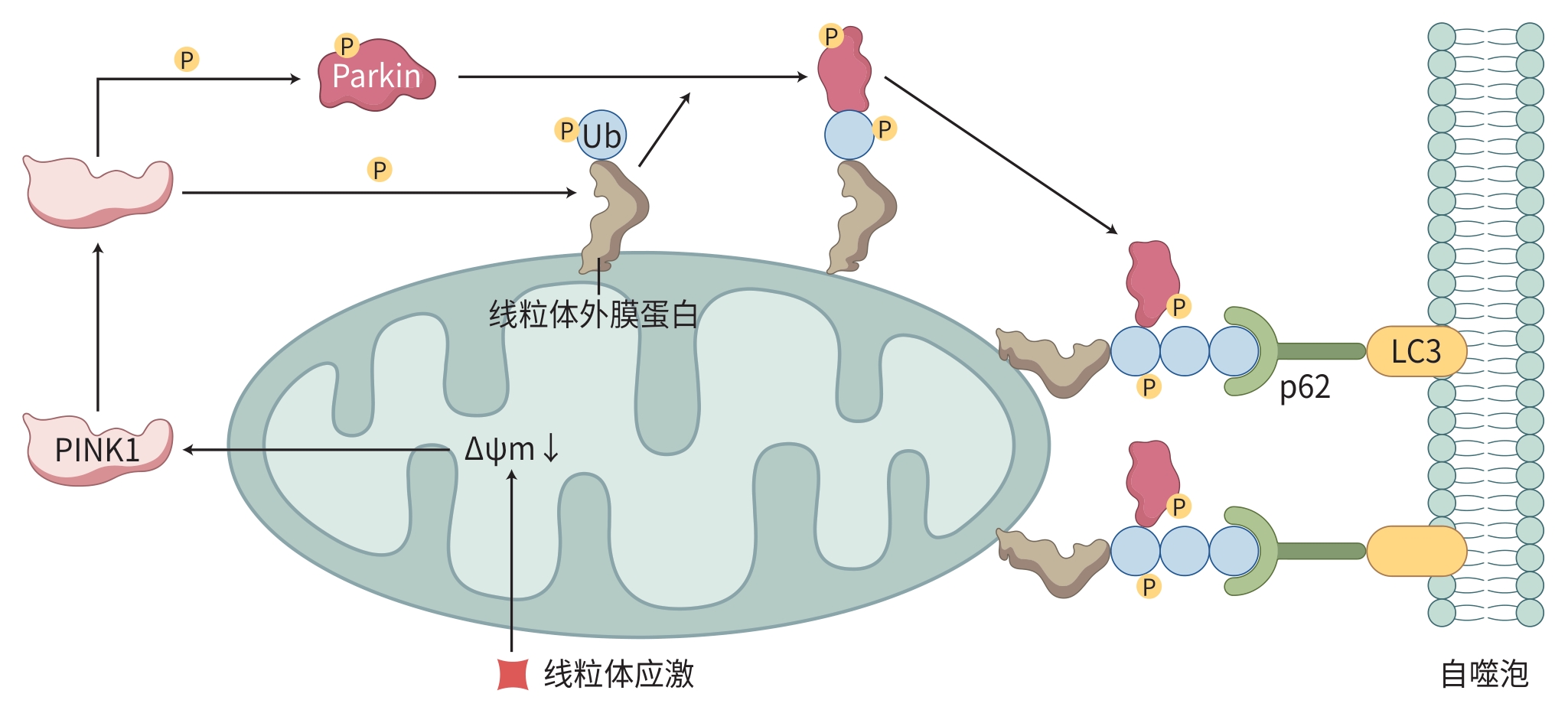
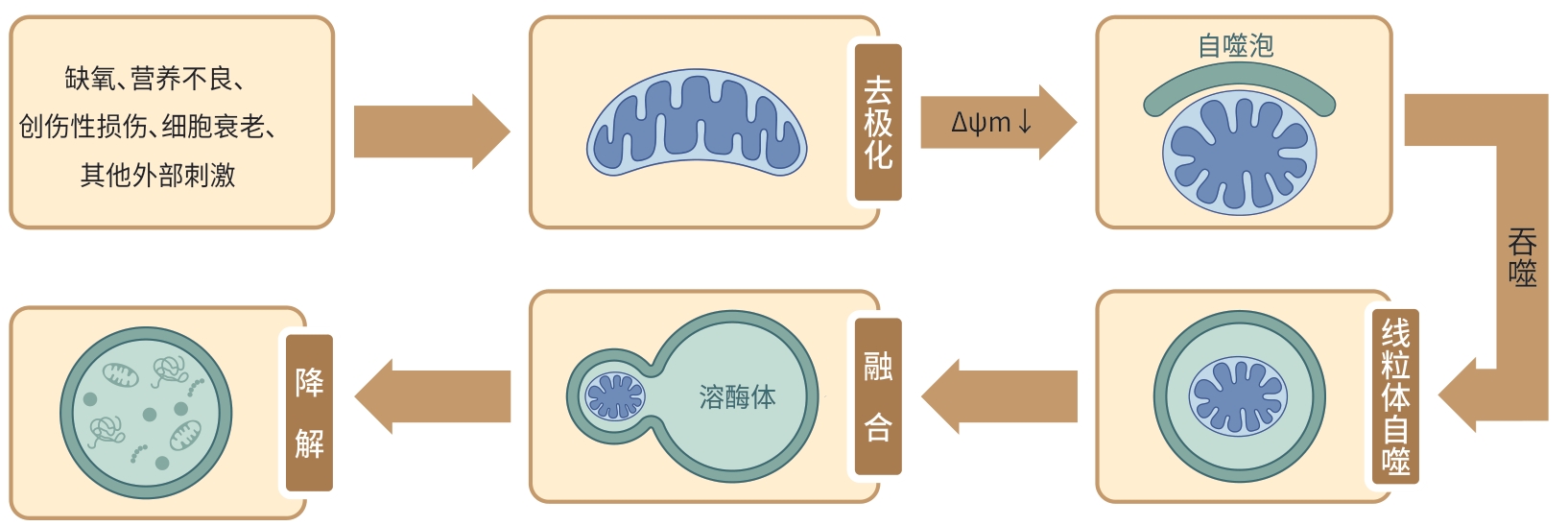
摘要: 代谢相关脂肪性肝病(MAFLD)发病机制复杂,而线粒体自噬参与了MAFLD的发生发展,在肝脏代谢途径和信号网络中起着关键作用。线粒体自噬受多种途径的调控,同源性磷酸酶张力蛋白诱导激酶1(PINK1)/帕金蛋白(Parkin)途径被认为是调节线粒体自噬的主要途径,PINK1/Parkin介导的线粒体自噬可调节脂质代谢、炎症及纤维化,缓解MAFLD的进展。本文综述了PINK1/Parkin介导的线粒体自噬在MAFLD中的作用及靶向治疗的研究进展,以期为防治MAFLD提供理论依据和思路。
-
关键词:
- 代谢相关脂肪性肝病 /
- 线粒体自噬 /
- PINK1/Parkin信号通路
Abstract: Metabolic associated fatty liver disease (MAFLD) has a complex pathogenesis, and mitophagy is involved in the development and progression of MAFLD and plays a key role in liver metabolic pathways and signaling networks. Mitophagy is regulated by a variety of pathways, and the PTEN-induced kinase 1 (PINK1)/Parkin pathway is considered the main pathway for regulating mitophagy. Mitophagy mediated by the PINK1/Parkin pathway can regulate lipid metabolism, inflammation, and fibrosis and delay the progression of MAFLD. This article reviews the role of mitophagy mediated by the PINK1/Parkin pathway in MAFLD and the research advances in targeted therapy, in order to provide theoretical bases and ideas for the prevention and treatment of MAFLD. -
[1] GOFTON C, UPENDRAN Y, ZHENG MH, et al. MAFLD: How is it different from NAFLD?[J]. Clin Mol Hepatol, 2023, 29( Suppl): S17- S31. DOI: 10.3350/cmh.2022.0367. [2] PIPITONE RM, CICCIOLI C, INFANTINO G, et al. MAFLD: A multisystem disease[J]. Ther Adv Endocrinol Metab, 2023, 14: 20420188221145549. DOI: 10.1177/20420188221145549. [3] ESLAM M, NEWSOME PN, SARIN SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement[J]. J Hepatol, 2020, 73( 1): 202- 209. DOI: 10.1016/j.jhep.2020.03.039. [4] ZHOU T, CHANG L, LUO Y, et al. Mst1 inhibition attenuates non-alcoholic fatty liver disease via reversing Parkin-related mitophagy[J]. Redox Biol, 2019, 21: 101120. DOI: 10.1016/j.redox.2019.101120. [5] LI W, JIANG WS, SU YR, et al. PINK1/Parkin-mediated mitophagy inhibits osteoblast apoptosis induced by advanced oxidation protein products[J]. Cell Death Dis, 2023, 14( 2): 88. DOI: 10.1038/s41419-023-05595-5. [6] LV TT, FAN XD, HE C, et al. SLC7A11-ROS/αKG-AMPK axis regulates liver inflammation through mitophagy and impairs liver fibrosis and NASH progression[J]. Redox Biol, 2024, 72: 103159. DOI: 10.1016/j.redox.2024.103159. [7] URBINA-VARELA R, CASTILLO N, VIDELA LA, et al. Impact of mitophagy and mitochondrial unfolded protein response as new adaptive mechanisms underlying old pathologies: Sarcopenia and non-alcoholic fatty liver disease[J]. Int J Mol Sci, 2020, 21( 20): 7704. DOI: 10.3390/ijms21207704. [8] ZHANG H, ZHANG Y, ZHAO WW, et al. PINK1/Parkin-mediated mitophagy and its mechanism of action in the development and progression of liver diseases[J]. J Clin Hepatol, 2020, 36( 7): 1663- 1665. DOI: 10.3969/j.issn.1001-5256.2020.07.048.张浩, 张悦, 赵文武, 等. PINK1/Parkin介导的线粒体自噬及其在肝脏疾病发生发展中的作用机制[J]. 临床肝胆病杂志, 2020, 36( 7): 1663- 1665. DOI: 10.3969/j.issn.1001-5256.2020.07.048. [9] WANG SL, LONG HJ, HOU LJ, et al. The mitophagy pathway and its implications in human diseases[J]. Signal Transduct Target Ther, 2023, 8( 1): 304. DOI: 10.1038/s41392-023-01503-7. [10] SCHMID ET, PYO JH, WALKER DW. Neuronal induction of BNIP3-mediated mitophagy slows systemic aging in Drosophila[J]. Nat Aging, 2022, 2( 6): 494- 507. DOI: 10.1038/s43587-022-00214-y. [11] ZHANG YH, WENG JJ, HUAN LY, et al. Mitophagy in atherosclerosis: From mechanism to therapy[J]. Front Immunol, 2023, 14: 1165507. DOI: 10.3389/fimmu.2023.1165507. [12] KATAYAMA H, HAMA H, NAGASAWA K, et al. Visualizing and modulating mitophagy for therapeutic studies of neurodegeneration[J]. Cell, 2020, 181( 5): 1176- 1187. e 16. DOI: 10.1016/j.cell.2020.04.025. [13] WU XL, ZHENG YR, LIU MR, et al. BNIP3L/NIX degradation leads to mitophagy deficiency in ischemic brains[J]. Autophagy, 2021, 17( 8): 1934- 1946. DOI: 10.1080/15548627.2020.1802089. [14] LU YY, LI ZJ, ZHANG SQ, et al. Cellular mitophagy: Mechanism, roles in diseases and small molecule pharmacological regulation[J]. Theranostics, 2023, 13( 2): 736- 766. DOI: 10.7150/thno.79876. [15] ZHANG T, LIU Q, GAO WH, et al. The multifaceted regulation of mitophagy by endogenous metabolites[J]. Autophagy, 2022, 18( 6): 1216- 1239. DOI: 10.1080/15548627.2021.1975914. [16] TEREŠAK P, LAPAO AN, SUBIC N, et al. Regulation of PRKN-independent mitophagy[J]. Autophagy, 2022, 18( 1): 24- 39. DOI: 10.1080/15548627.2021.1888244. [17] WANG ZT, CHAN SW, ZHAO H, et al. Outlook of PINK1/Parkin signaling in molecular etiology of Parkinson’s disease, with insights into Pink1 knockout models[J]. Zool Res, 2023, 44( 3): 559- 576. DOI: 10.24272/j.issn.2095-8137.2022.406. [18] QIU YX, XU J, CHEN YL, et al. Parkin plays a crucial role in acute viral myocarditis by regulating mitophagy activity[J]. Theranostics, 2024, 14( 13): 5303- 5315. DOI: 10.7150/thno.97675. [19] WADE HARPER J, ORDUREAU A, HEO JM. Building and decoding ubiquitin chains for mitophagy[J]. Nat Rev Mol Cell Biol, 2018, 19( 2): 93- 108. DOI: 10.1038/nrm.2017.129. [20] ZHAO XP, WANG Z, WANG LJ, et al. The PINK1/Parkin signaling pathway-mediated mitophagy: A forgotten protagonist in myocardial ischemia/reperfusion injury[J]. Pharmacol Res, 2024, 209: 107466. DOI: 10.1016/j.phrs.2024.107466. [21] SAUVÉ V, STEFAN E, CROTEAU N, et al. Activation of parkin by a molecular glue[J]. Nat Commun, 2024, 15( 1): 7707. DOI: 10.1038/s41467-024-51889-3. [22] MARTINEZ A, SANCHEZ-MARTINEZ A, PICKERING JT, et al. Mitochondrial CISD1/Cisd accumulation blocks mitophagy and genetic or pharmacological inhibition rescues neurodegenerative phenotypes in Pink1/parkin models[J]. Mol Neurodegener, 2024, 19( 1): 12. DOI: 10.1186/s13024-024-00701-3. [23] JIN ZZ, CHANG BH, WEI YL, et al. Curcumin exerts chondroprotective effects against osteoarthritis by promoting AMPK/PINK1/Parkin-mediated mitophagy[J]. Biomed Pharmacother, 2022, 151: 113092. DOI: 10.1016/j.biopha.2022.113092. [24] ZHANG YX, WANG Y, YOU CL, et al. Analysis of factors associated with abnormal liver function in patients with non-alcoholic fatty liver disease[J]. Clin J Med Offic, 2025, 53( 5): 522- 524, 528. DOI: 10.16680/j.1671-3826.2025.05.21.张月霞, 王宇, 尤丛蕾, 等. 非酒精性脂肪肝患者肝功能异常相关因素分析[J]. 临床军医杂志, 2025, 53( 5): 522- 524, 528. DOI: 10.16680/j.1671-3826.2025.05.21. [25] DI CIAULA A, PASSARELLA S, SHANMUGAM H, et al. Nonalcoholic fatty liver disease(NAFLD). mitochondria as players and targets of therapies?[J]. Int J Mol Sci, 2021, 22( 10): 5375. DOI: 10.3390/ijms22105375. [26] WANG DH, JIANG SW, HU AR, et al. Mulberry exerts antioxidant stress effect in rats with nonalcoholic fatty liver disease[J]. Chin J Clin Pharmacol Ther, 2023, 28( 6): 609- 616. DOI: 10.12092/j.issn.1009-2501.2023.06.002.汪东辉, 蒋素文, 胡爱荣, 等. 桑葚改善大鼠非酒精性脂肪性肝病的氧化应激损伤[J]. 中国临床药理学与治疗学, 2023, 28( 6): 609- 616. DOI: 10.12092/j.issn.1009-2501.2023.06.002. [27] ZHAO Y, ZHOU YN, WANG D, et al. Mitochondrial dysfunction in metabolic dysfunction fatty liver disease(MAFLD)[J]. Int J Mol Sci, 2023, 24( 24): 17514. DOI: 10.3390/ijms242417514. [28] ZHENG YW, WANG ST, WU JL, et al. Mitochondrial metabolic dysfunction and non-alcoholic fatty liver disease: New insights from pathogenic mechanisms to clinically targeted therapy[J]. J Transl Med, 2023, 21( 1): 510. DOI: 10.1186/s12967-023-04367-1. [29] MA XW, MCKEEN T, ZHANG JH, et al. Role and mechanisms of mitophagy in liver diseases[J]. Cells, 2020, 9( 4): 837. DOI: 10.3390/cells9040837. [30] UNDAMATLA R, FAGUNLOYE OG, CHEN J, et al. Reduced mitophagy is an early feature of NAFLD and liver-specific PARKIN knockout hastens the onset of steatosis, inflammation and fibrosis[J]. Sci Rep, 2023, 13( 1): 7575. DOI: 10.1038/s41598-023-34710-x. [31] HE H, TANG Y, ZHUANG L, et al. PINK1/Park2-mediated mitophagy relieve non-alcoholic fatty liver disease[J]. Physiol Res, 2024, 73( 2): 253- 263. DOI: 10.33549/physiolres.934925. [32] ZHANG Y, WANG ZY, JIA CY, et al. Blockade of hepatocyte PCSK9 ameliorates hepatic ischemia-reperfusion injury by promoting Pink1-parkin-mediated mitophagy[J]. Cell Mol Gastroenterol Hepatol, 2024, 17( 1): 149- 169. DOI: 10.1016/j.jcmgh.2023.09.004. [33] ZHANG ZH. The deletion of glycogen synthase kinase 3β in macrophages alleviates the progress of nonalcoholic steatohepatitis by promoting mitochondrial autophagy mediated by PINK1[D]. Nanjing: Nanjing Medical University, 2023.张子豪. 巨噬细胞中糖原合成酶激酶3β缺失通过促进PINK1介导的线粒体自噬缓解非酒精性脂肪性肝炎的进展[D]. 南京: 南京医科大学, 2023. [34] ZHANG NP, LIU XJ, XIE L, et al. Impaired mitophagy triggers NLRP3 inflammasome activation during the progression from nonalcoholic fatty liver to nonalcoholic steatohepatitis[J]. Lab Invest, 2019, 99( 6): 749- 763. DOI: 10.1038/s41374-018-0177-6. [35] DING Q, XIE XL, WANG MM, et al. The role of the apoptosis-related protein BCL-B in the regulation of mitophagy in hepatic stellate cells during the regression of liver fibrosis[J]. Exp Mol Med, 2019, 51( 1): 1- 13. DOI: 10.1038/s12276-018-0199-6. [36] SEMMLER G, DATZ C, REIBERGER T, et al. Diet and exercise in NAFLD/NASH: Beyond the obvious[J]. Liver Int, 2021, 41( 10): 2249- 2268. DOI: 10.1111/liv.15024. [37] YANG B, ZHANG R. Progress on the treatment of metabolic associated fatty liver disease[J/CD]. Chin J Liver Dis(Electronic Version), 2024, 16( 4): 25- 30. DOI: 10.3969/j.issn.1674-7380.2024.04.004.杨彬, 张瑞. 代谢相关脂肪性肝病治疗进展[J/CD]. 中国肝脏病杂志(电子版), 2024, 16( 4): 25- 30. DOI: 10.3969/j.issn.1674-7380.2024.04.004. [38] LI GL, LIU XL, MIAO ZF, et al. Preparation of corn peptides with anti-adhesive activity and its functionality to alleviate gastric injury induced by Helicobacter pylori infection in vivo[J]. Nutrients, 2023, 15( 15): 3467. DOI: 10.3390/nu15153467. [39] YAO ZC, LI XL, WANG WT, et al. Corn peptides attenuate non-alcoholic fatty liver disease via PINK1/Parkin-mediated mitochondrial autophagy[J]. Food Nutr Res, 2023, 67: 67. DOI: 10.29219/fnr.v67.9547. [40] ZOU YY, TANG XB, CHEN ZL, et al. Exercise intervention improves mitochondrial quality in non-alcoholic fatty liver disease zebrafish[J]. Front Endocrinol(Lausanne), 2023, 14: 1162485. DOI: 10.3389/fendo.2023.1162485. [41] GAO Y, ZHANG W, ZENG LQ, et al. Exercise and dietary intervention ameliorate high-fat diet-induced NAFLD and liver aging by inducing lipophagy[J]. Redox Biol, 2020, 36: 101635. DOI: 10.1016/j.redox.2020.101635. [42] ROSA-CALDWELL ME, POOLE KE, SEIJA A, et al. Exercise during weight loss improves hepatic mitophagy[J]. Sports Med Health Sci, 2022, 4( 3): 183- 189. DOI: 10.1016/j.smhs.2022.04.003. [43] SANJAY, SHIN JH, PARK M, et al. Cyanidin-3-O-glucoside regulates the M1/M2 polarization of microglia via PPARγ and Aβ42 phagocytosis through TREM2 in an Alzheimer's disease model[J]. Mol Neurobiol, 2022, 59( 8): 5135- 5148. DOI: 10.1007/s12035-022-02873-9. [44] LI XW, SHI Z, ZHU YW, et al. Cyanidin-3-O-glucoside improves non-alcoholic fatty liver disease by promoting PINK1-mediated mitophagy in mice[J]. Br J Pharmacol, 2020, 177( 15): 3591- 3607. DOI: 10.1111/bph.15083. [45] GENG YN, WU ZM, BUIST-HOMAN M, et al. Hesperetin protects against palmitate-induced cellular toxicity via induction of GRP78 in hepatocytes[J]. Toxicol Appl Pharmacol, 2020, 404: 115183. DOI: 10.1016/j.taap.2020.115183. [46] LI W, CAI ZN, SCHINDLER F, et al. Elevated PINK1/parkin-dependent mitophagy and boosted mitochondrial function mediate protection of HepG2 cells from excess palmitic acid by hesperetin[J]. J Agric Food Chem, 2024, 72( 23): 13039- 13053. DOI: 10.1021/acs.jafc.3c09132. [47] SUN DQ, ZHOU XL, WU T, et al. Study on the mechanism of action of Lizhong Tang in ameliorating non-alcoholic fatty liver disease by regulating mitochondrial autophagy[J]. J Hainan Med Univ, 2023, 29( 21): 1614- 1619. DOI: 10.13210/j.cnki.jhmu.20231009.001.孙东琪, 周晓玲, 吴腾, 等. 理中汤通过调控线粒体自噬改善非酒精性脂肪性肝病的作用机制研究[J]. 海南医学院学报, 2023, 29( 21): 1614- 1619. DOI: 10.13210/j.cnki.jhmu.20231009.001. [48] ZHOU ZJ. Based on mitochondrial autophagy PINK1/Parkin signaling pathway, the mechanism of Zaozhuyinchen recipe in treating nonalcoholic steatohepatitis in rats was discussed[D]. Xiamen: Xiamen University, 2021.周志佳. 基于线粒体自噬PINK1/Parkin信号通路探讨皂术茵陈方治疗大鼠非酒精性脂肪性肝炎的作用机制[D]. 厦门: 厦门大学, 2021. [49] JI BHXM, ZHANG YR, CHEN XL, et al. Study on the mechanism of Qutan Huoxue Recipe regulating PINK1/Parkin signaling pathway to induce autophagy of NASH rat hepatocytes[J]. Chin J Integr Tradit West Med Liver Dis, 2023, 33( 8): 710- 715. DOI: 10.3969/j.issn.1005-0264.2023.008.008.吉布和学莫, 张玉蓉, 陈相霖, 等. 祛痰活血方调控PINK1/Parkin信号通路诱导NASH大鼠肝细胞自噬的实验研究[J]. 中西医结合肝病杂志, 2023, 33( 8): 710- 715. DOI: 10.3969/j.issn.1005-0264.2023.008.008. [50] POPOVICIU MS, PĂDURARU L, YAHYA G, et al. Emerging role of GLP-1 agonists in obesity: a comprehensive review of randomised controlled trials[J]. Int J Mol Sci, 2023, 24( 13): 10449. DOI: 10.3390/ijms241310449. [51] SHAO N, YU XY, MA XF, et al. Exenatide delays the progression of nonalcoholic fatty liver disease in C57BL/6 mice, which may involve inhibition of the NLRP3 inflammasome through the mitophagy pathway[J]. Gastroenterol Res Pract, 2018, 2018: 1864307. DOI: 10.1155/2018/1864307. [52] YU XY, HAO M, LIU Y, et al. Liraglutide ameliorates non-alcoholic steatohepatitis by inhibiting NLRP3 inflammasome and pyroptosis activation via mitophagy[J]. Eur J Pharmacol, 2019, 864: 172715. DOI: 10.1016/j.ejphar.2019.172715. -



 PDF下载 ( 1212 KB)
PDF下载 ( 1212 KB)

 下载:
下载: