新型简化胰岛素抵抗指标对脂肪胰发生风险的预测价值
DOI: 10.12449/JCH250824
The predictive value of new simplified insulin resistance assessment indicators for the development of fatty pancreatic disease
-
摘要:
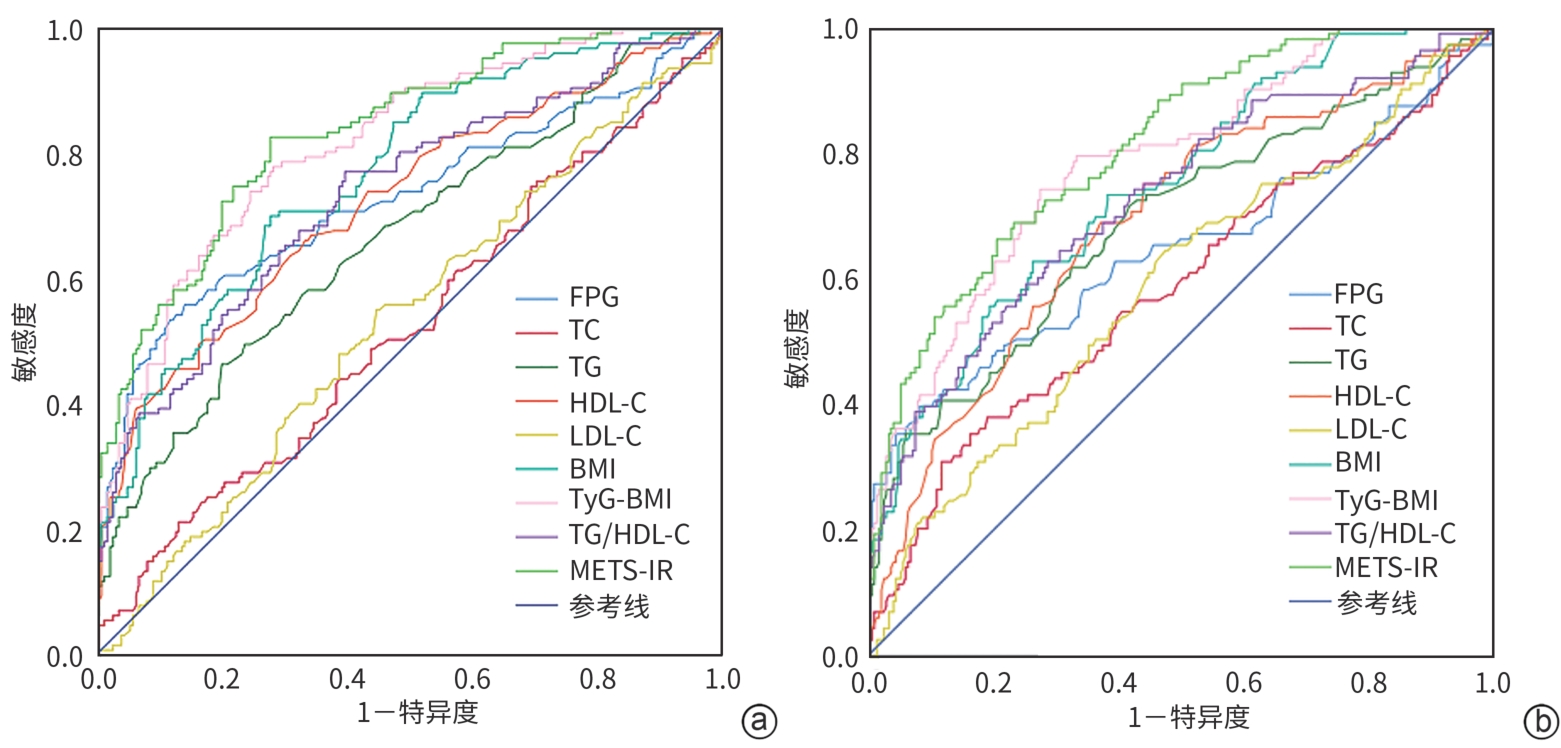
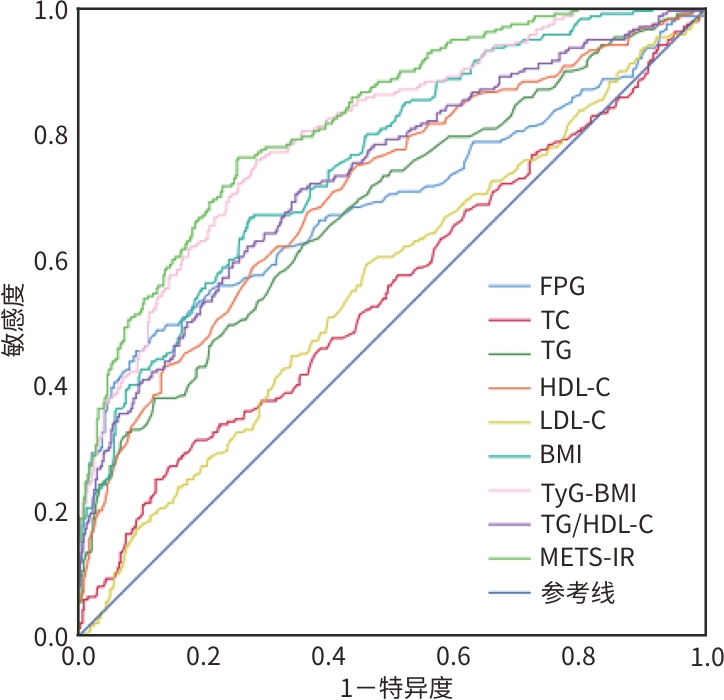
目的 探讨三酰甘油葡萄糖-体质量指数(TyG-BMI)、血清三酰甘油/高密度脂蛋白胆固醇(TG/HDL-C)及胰岛素抵抗代谢评分(METS-IR)对脂肪胰的预测价值。 方法 纳入于2020年1月—2023年11月在郑州大学第一附属医院就诊的240例脂肪胰患者为脂肪胰组,同时随机选取同期健康体检者480例作为对照组。收集受试者的一般临床资料和实验室相关指标等数据。计量资料非正态分布两组间比较采用Mann-Whitney U秩和检验。计数资料两组间比较采用χ2检验。采用二元Logistic回归探讨TyG-BMI、TG/HDL-C以及METS-IR与脂肪胰的关系。绘制受试者操作特征曲线(ROC曲线),计算曲线下面积(AUC)评估各简化胰岛素抵抗指标对总人群及不同性别人群脂肪胰的预测诊断价值。 结果 脂肪胰组的年龄、BMI、收缩压(SBP)、舒张压(DBP)、空腹血糖(FPG)、血尿酸(SUA)、ALT、AST、GGT、TC、TG、LDL-C、TyG-BMI、TG/HDL-C、METS-IR,以及高血压史、糖尿病史和脂肪肝比例均显著高于对照组(P值均<0.05)。而HDL-C水平显著低于对照组(P<0.05)。多因素Logistic回归分析结果显示,在调整各影响因素后,TyG-BMI、TG/HDL-C及METS-IR仍是脂肪胰发生的独立危险因素(OR分别为1.027、6.964、1.184,95%CI分别为1.018~1.037、2.022~23.989、1.123~1.248)。ROC曲线分析表明,METS-IR、TyG-BMI的AUC分别为0.823、0.803,敏感度为76.3%、75.8%,特异度为74.6%、71.7%,最佳临界值为34.86、196.70。其次为BMI(AUC=0.758)及TG/HDL-C(AUC=0.734)。在性别分层分析中,男性和女性亚组中METS-IR的AUC值均为最高,分别为0.834、0.810。 结论 TyG-BMI、TG/HDL-C及METS-IR对脂肪胰的发生均有良好的预测价值,其中METS-IR的预测效能更佳。 Abstract:Objective To investigate the predictive value of triglyceride glucose-body mass index (TyG-BMI), serum triglyceride-to-high-density lipoprotein cholesterol ratio (TG/HDL-C), and metabolic score for insulin resistance (METS-IR) for fatty pancreatic disease (FPD). Methods A total of 240 patients with FPD treated in The First Affiliated Hospital of Zhengzhou University from January 2020 to November 2023 were included as the case group, while 480 healthy subjects who underwent healthy checks in the same period were randomly selected as the control group. General clinical data and laboratory indicators were collected. The Mann-Whitney U test and chi-square test were used to compare non-normally distributed continuous variables, and categorical variables between groups, respectively. A binary logistic regression model was used to assess the relationship between TyG-BMI, TG/HDL-C, and METS-IR and FPD. The receiver operating characteristic (ROC) curve was plotted, and the area under the curve (AUC) was calculated to evaluate the predictive diagnostic value of those simplified insulin resistance indicators for FPD in the general population and different sex populations. Results Age, BMI, systolic blood pressure, diastolic blood pressure, fasting plasma glucose, uric acid, alanine aminotransferase, aspartate aminotransferase, gamma-glutamyl transferase, total cholesterol, triglyceride, low-density lipoprotein cholesterol, TyG-BMI, TG/HDL-C, and METS-IR in the case group were significantly higher than those in the control group (all P<0.05). The case group had significantly higher proportions of individuals with hypertension, diabetes, and fatty liver disease than the control group (all P<0.05). The high-density lipoprotein cholesterol level was significantly lower in the case group than in the control group (P<0.05). The multivariable Logistic regression analysis showed that after adjusting for various influencing factors, TyG-BMI, TG/HDL-C, and METS-IR remained as independent risk factors for the development of FPD, with the odds ratios (95% confidence intervals) being 1.027 (1.018 — 1.037), 6.964(2.022 — 23.989), and 1.184 (1.123 — 1.248), respectively. In the ROC curve analysis, the AUCs of METS-IR and TyG-BMI were 0.823 and 0.803, respectively, with their sensitivities being 76.3% and 75.8%, specificities being 74.6% and 71.7%, and optimal cut-off values being 34.86 and 196.70, respectively; the next were BMI (AUC=0.758) and TG/HDL-C (AUC=0.734); in the sex-stratified analysis, the AUC values of METS-IR were highest in both the male and female subgroups, which were 0.834 and 0.810, respectively. Conclusion TyG-BMI, TG/HDL-C, and METS-IR show good predictive value for the development of FPD, in which METS-IR is more excellent. -
Key words:
- Pancreatic Diseases /
- Insulin Resistance /
- Diagnosis
-
表 1 受试者基线资料分析
Table 1. Analysis of subjects’ baseline data
指标 脂肪胰组(n=240) 对照组(n=480) 统计值 P值 男[例(%)] 127(52.9) 219(45.6) χ2=3.408 0.065 年龄(岁) 62.00(54.25~72.00) 50.00(36.00~59.00) Z=-10.595 <0.001 BMI(kg/m2) 25.06(23.06~27.74) 22.49(20.45~24.24) Z=-11.285 <0.001 吸烟史[例(%)] 26(10.8) 35(7.3) χ2=2.588 0.108 饮酒史[例(%)] 17(7.1) 22(4.6) χ2=1.952 0.162 高血压史[例(%)] 100(41.7) 122(25.4) χ2=19.811 <0.001 糖尿病史[例(%)] 82(34.2) 25(5.2) χ2=106.044 <0.001 脂肪肝[例(%)] 95(39.6) 67(14.0) χ2=60.251 <0.001 SBP(mmHg) 125.50(120.00~135.75) 122.00(113.00~135.00) Z=-3.943 <0.001 DBP(mmHg) 77.50(71.00~84.00) 76.00(69.00~84.00) Z=-2.392 0.017 FPG(mmol/L) 5.31(4.57~6.86) 4.75(4.37~5.12) Z=-8.345 <0.001 SUA(μmol/L) 294.50(224.50~369.00) 267.50(219.25~326.50) Z=-2.872 0.004 ALT(U/L) 16.00(11.00~26.00) 14.00(10.00~19.00) Z=-3.900 <0.001 AST(U/L) 19.00(15.00~24.00) 18.00(15.00~21.00) Z=-2.432 0.015 GGT(U/L) 22.00(14.25~35.75) 14.00(11.00~20.00) Z=-8.724 <0.001 TC(mmol/L) 4.49(3.85~5.44) 4.35(3.71~4.97) Z=-2.199 0.028 TG(mmol/L) 1.21(0.89~1.76) 0.91(0.71~1.21) Z=-7.924 <0.001 HDL-C(mmol/L) 1.06(0.86~1.28) 1.31(1.08~1.60) Z=-9.114 <0.001 LDL-C(mmol/L) 2.85(2.24~3.52) 2.66(2.14~3.24) Z=-2.618 0.009 TyG-BMI 217.23(196.77~242.73) 183.58(164.39~201.44) Z=-13.259 <0.001 TG/HDL-C 1.18(0.77~1.92) 0.70(0.46~1.03) Z=-10.232 <0.001 METS-IR 39.54(35.04~46.22) 31.69(27.85~35.19) Z=-14.159 <0.001 表 2 单因素Logistic回归分析FPD发生的影响因素
Table 2. The univariate Logistic regression analysis of the factors of influencing the occurrence of FPD
项目 β值 P值 OR 95%CI 年龄 0.060 <0.001 1.062 1.049~1.076 高血压史 0.740 <0.001 2.096 1.509~2.912 糖尿病史 2.246 <0.001 9.446 5.827~15.31 脂肪肝 1.396 <0.001 4.039 2.802~5.820 BMI 0.339 <0.001 1.403 1.317~1.495 SBP 0.018 <0.001 1.019 1.009~1.028 DBP 0.017 0.011 1.017 1.004~1.031 FPG 0.731 <0.001 2.077 1.744~2.473 SUA 0.003 0.001 1.003 1.001~1.005 ALT 0.031 <0.001 1.031 1.018~1.045 AST 0.034 <0.001 1.034 1.015~1.054 GGT 0.040 <0.001 1.041 1.030~1.052 TC 0.207 0.008 1.231 1.057~1.433 TG 1.374 <0.001 3.950 2.816~5.542 HDL-C -2.059 <0.001 0.128 0.077~0.212 LDL-C -0.006 0.671 0.995 0.970~1.020 TyG-BMI 0.039 <0.001 1.040 1.033~1.047 TG/HDL-C 1.393 <0.001 4.027 2.983~5.436 METS-IR 0.202 <0.001 1.224 1.184~1.266 表 3 总人群各指标预测脂肪胰的ROC曲线分析
Table 3. ROC
curve analysis of FPD prediction with different indexes in total population 项目 AUC 95%CI 敏感度(%) 特异度(%) 最大约登指数 临界值 FPG 0.691 0.645~0.736 48.8 87.5 0.363 5.40 TC 0.550 0.504~0.596 25.0 87.7 0.127 5.45 TG 0.681 0.639~0.723 62.5 64.2 0.267 1.07 HDL-C 0.708 0.667~0.749 58.8 72.3 0.311 1.12 LDL-C 0.560 0.515~0.605 59.2 54.2 0.134 2.73 BMI 0.758 0.721~0.794 66.7 72.7 0.394 23.91 TyG-BMI 0.803 0.769~0.836 75.8 71.7 0.475 196.70 TG/HDL-C 0.734 0.694~0.773 71.3 64.6 0.359 0.85 METS-IR 0.823 0.792~0.855 76.3 74.6 0.509 34.86 表 4 不同性别亚组各指标预测脂肪胰的ROC曲线分析
Table 4. ROC
curve analysis of fatty pancreatic disease prediction using various indexes across different gender 项目 AUC 95%CI 敏感度(%) 特异度(%) 最大约登指数 临界值 男性 FPG 0.728 0.668~0.788 55.9 85.8 0.417 5.36 TC 0.525 0.461~0.589 21.3 86.8 0.081 5.35 TG 0.667 0.607~0.726 46.5 79.9 0.264 1.28 HDL-C 0.722 0.665~0.779 49.6 83.6 0.332 1.01 LDL-C 0.535 0.472~0.598 55.1 55.3 0.104 2.73 BMI 0.768 0.717~0.818 70.1 72.1 0.422 23.91 TyG-BMI 0.817 0.771~0.862 78.0 71.7 0.497 197.70 TG/HDL-C 0.734 0.678~0.789 77.2 60.3 0.375 0.85 METS-IR 0.834 0.791~0.878 82.7 72.1 0.548 34.91 女性 FPG 0.649 0.581~0.717 39.8 91.6 0.314 5.54 TC 0.587 0.521~0.653 31.0 88.1 0.191 5.45 TG 0.690 0.628~0.751 71.7 58.2 0.299 0.96 HDL-C 0.691 0.632~0.750 69.0 62.8 0.318 0.78 LDL-C 0.590 0.525~0.654 64.6 52.5 0.171 2.72 BMI 0.746 0.693~0.799 62.8 73.6 0.364 23.97 TyG-BMI 0.787 0.737~0.837 74.3 72.4 0.467 195.75 TG/HDL-C 0.726 0.668~0.783 62.8 71.3 0.341 0.89 METS-IR 0.810 0.765~0.856 66.4 79.3 0.457 35.67 -
[1] PETROV MS, TAYLOR R. Intra-pancreatic fat deposition: Bringing hidden fat to the fore[J]. Nat Rev Gastroenterol Hepatol, 2022, 19( 3): 153- 168. DOI: 10.1038/s41575-021-00551-0. [2] SHAH N, ROCHA JP, BHUTIANI N, et al. Nonalcoholic fatty pancreas disease[J]. Nutr Clin Pract, 2019, 34( Suppl 1): S49- S56. DOI: 10.1002/ncp.10397. [3] WAGNER R, ECKSTEIN SS, YAMAZAKI H, et al. Metabolic implications of pancreatic fat accumulation[J]. Nat Rev Endocrinol, 2022, 18( 1): 43- 54. DOI: 10.1038/s41574-021-00573-3. [4] KOÇ U, TAYDAŞ O. Evaluation of pancreatic steatosis prevalence and anthropometric measurements using non-contrast computed tomography[J]. Turk J Gastroenterol, 2020, 31( 9): 640- 648. DOI: 10.5152/tjg.2020.19434. [5] LIPP M, TARJÁN D, LEE JM, et al. Fatty pancreas is a risk factor for pancreatic cancer: A systematic review and meta-analysis of 2956 patients[J]. Cancers(Basel), 2023, 15( 19): 4876. DOI: 10.3390/cancers15194876. [6] LI RR, SHI XW, CHEN W, et al. A comparative study on the predictive value of new simplified insulin resistance assessment indicators in identifying glucose metabolism disturbance[J]. Chin J Diabetes Mellitus, 2022, 14( 1): 56- 62. DOI: 10.3760/cma.j.cn115791-20210805-00428.李融融, 时小东, 陈伟, 等. 新型简化胰岛素抵抗评价指标对糖代谢紊乱预测价值的比较研究[J]. 中华糖尿病杂志, 2022, 14( 1): 56- 62. DOI: 10.3760/cma.j.cn115791-20210805-00428. [7] LEE JH, PARK K, LEE HS, et al. The usefulness of metabolic score for insulin resistance for the prediction of incident non-alcoholic fatty liver disease in Korean adults[J]. Clin Mol Hepatol, 2022, 28( 4): 814- 826. DOI: 10.3350/cmh.2022.0099. [8] ZENG P, CAI XS, YU XZ, et al. Markers of insulin resistance associated with non-alcoholic fatty liver disease in non-diabetic population[J]. Sci Rep, 2023, 13( 1): 20470. DOI: 10.1038/s41598-023-47269-4. [9] LI XT, SUN MZ, YANG YX, et al. Predictive effect of triglyceride glucose-related parameters, obesity indices, and lipid ratios for diabetes in a Chinese population: A prospective cohort study[J]. Front Endocrinol(Lausanne), 2022, 13: 862919. DOI: 10.3389/fendo.2022.862919. [10] JIANG R, LI YX. Value of triglyceride-glucose index combined with obesity index in predicting nonalcoholic fatty liver disease in individuals with obstructive sleep apnea[J]. J Clin Hepatol, 2023, 39( 3): 546- 551. DOI: 10.3969/j.issn.1001-5256.2023.03.010.蒋绒, 李永霞. 甘油三酯葡萄糖乘积指数联合肥胖指标对阻塞性睡眠呼吸暂停患者发生非酒精性脂肪性肝病的预测价值[J]. 临床肝胆病杂志, 2023, 39( 3): 546- 551. DOI: 10.3969/j.issn.1001-5256.2023.03.010. [11] YUGE H, OKADA H, HAMAGUCHI M, et al. Triglycerides/HDL cholesterol ratio and type 2 diabetes incidence: Panasonic Cohort Study 10[J]. Cardiovasc Diabetol, 2023, 22( 1): 308. DOI: 10.1186/s12933-023-02046-5. [12] YAO J, XU R, LIU XN. Research progress of clinical importance of nonalcoholic fatty pancreas disease[J]. Chin J Pancreatol, 2019, 19( 1): 73- 77. DOI: 10.3760/cma.j.issn.1674-1935.2019.01.019.姚洁, 徐蓉, 刘歆农. 非酒精性脂肪性胰腺疾病临床意义的研究进展[J]. 中华胰腺病杂志, 2019, 19( 1): 73- 77. DOI: 10.3760/cma.j.issn.1674-1935.2019.01.019. [13] National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association; Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007.中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 临床肝胆病杂志, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. [14] REVISION JCFG. 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of Chinese guidelines for prevention and treatment of hypertension[J]. J Geriatr Cardiol, 2019, 16( 3): 182- 241. DOI: 10.11909/j.issn.1671-5411.2019.03.014. [15] Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China(2020 edition)[J]. Chin J Diabetes Mellit, 2021, 13( 4): 315- 409. DOI: 10.3760/cma.j.cn115791-20210221-00095.中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020年版)[J]. 中华糖尿病杂志, 2021, 13( 4): 315- 409. DOI: 10.3760/cma.j.cn115791-20210221-00095. [16] CHEN K, SHEN ZW, GU WJ, et al. Prevalence of obesity and associated complications in China: A cross-sectional, real-world study in 15.8 million adults[J]. Diabetes Obes Metab, 2023, 25( 11): 3390- 3399. DOI: 10.1111/dom.15238. [17] AHMED B, SULTANA R, GREENE MW. Adipose tissue and insulin resistance in obese[J]. Biomed Pharmacother, 2021, 137: 111315. DOI: 10.1016/j.biopha.2021.111315. [18] ZENG YY, YU J, ZHANG J, et al. Ultrasound quantitative evaluation of the correlation between pancreatic echo enhancement and dyslipidemia[J]. Chin J Med Offic, 2023, 51( 3): 258- 260, 265. DOI: 10.16680/j.1671-3826.2023.03.10.曾媛媛, 于晶, 张筠, 等. 超声定量评估胰腺回声增强与血脂异常相关性研究[J]. 临床军医杂志, 2023, 51( 3): 258- 260, 265. DOI: 10.16680/j.1671-3826.2023.03.10. [19] DONG XW, ZHU QT, YUAN CC, et al. Associations of intrapancreatic fat deposition with incident diseases of the exocrine and endocrine pancreas: A UK biobank prospective cohort study[J]. Am J Gastroenterol, 2024, 119( 6): 1158- 1166. DOI: 10.14309/ajg.0000000000002792. [20] CHIYANIKA C, CHAN DFY, HUI SCN, et al. The relationship between pancreas steatosis and the risk of metabolic syndrome and insulin resistance in Chinese adolescents with concurrent obesity and non-alcoholic fatty liver disease[J]. Pediatr Obes, 2020, 15( 9): e12653. DOI: 10.1111/ijpo.12653. [21] LEE JS, KIM SH, JUN DW, et al. Clinical implications of fatty pancreas: Correlations between fatty pancreas and metabolic syndrome[J]. World J Gastroenterol, 2009, 15( 15): 1869- 1875. DOI: 10.3748/wjg.15.1869. [22] LU T, WANG Y, DOU T, et al. Pancreatic fat content is associated with β-cell function and insulin resistance in Chinese type 2 diabetes subjects[J]. Endocr J, 2019, 66( 3): 265- 270. DOI: 10.1507/endocrj.EJ18-0436. [23] ROH E, KIM KM, PARK KS, et al. Comparison of pancreatic volume and fat amount linked with glucose homeostasis between healthy Caucasians and Koreans[J]. Diabetes Obes Metab, 2018, 20( 11): 2642- 2652. DOI: 10.1111/dom.13447. [24] OWEI I, JAIN N, JONES D, et al. Physiology of glycemic recovery and stabilization after hyperinsulinemic euglycemic clamp in healthy subjects[J]. J Clin Endocrinol Metab, 2018, 103( 11): 4155- 4162. DOI: 10.1210/jc.2018-01569. [25] XIAO Y, WANG H, HAN LN, et al. Predictive value of anthropometric and biochemical indices in non-alcoholic fatty pancreas disease: A cross-sectional study[J]. BMJ Open, 2024, 14( 4): e081131. DOI: 10.1136/bmjopen-2023-081131. -



 PDF下载 ( 1346 KB)
PDF下载 ( 1346 KB)

 下载:
下载: