960例不明原因肝病患者经肝活检病理诊断的病因构成与临床特征分析
DOI: 10.12449/JCH250823
Analysis of etiological composition and clinical characteristics in 960 cases of unexplained liver disease diagnosed by liver biopsy
-
摘要:
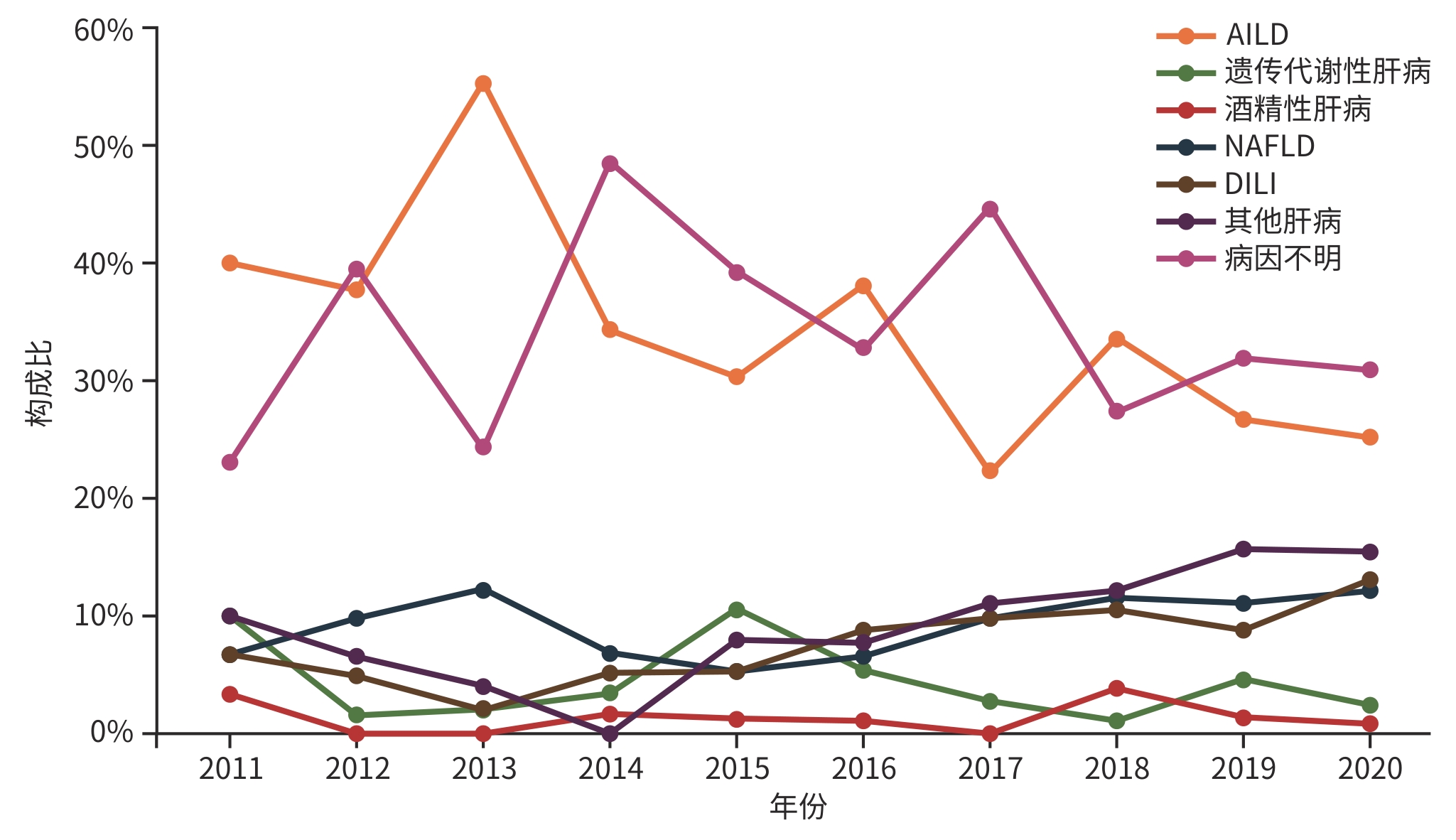
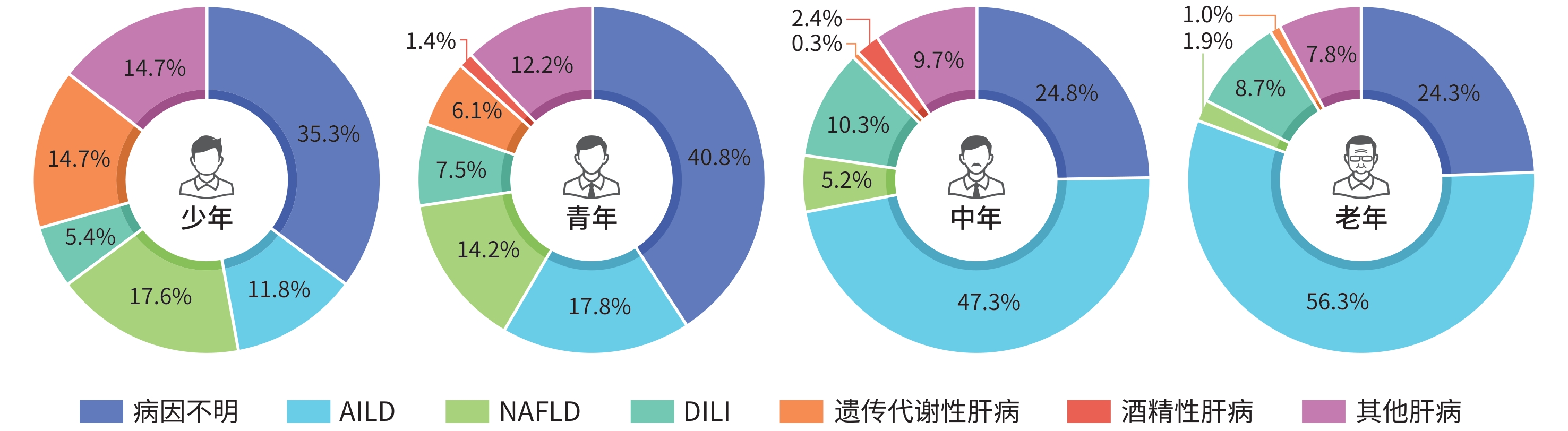
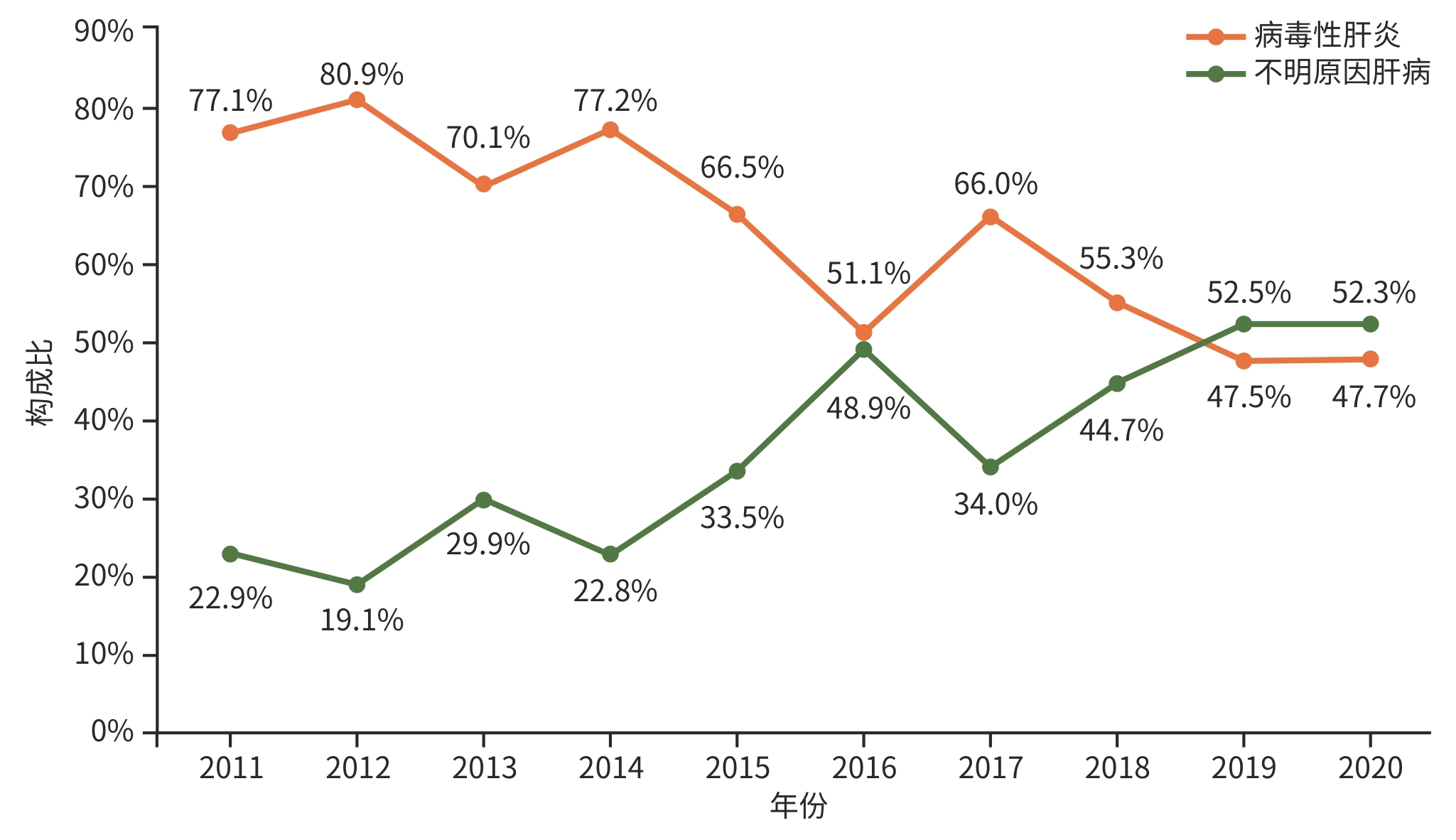
目的 了解不明原因肝病患者经肝活检后明确病因的构成比及趋势。 方法 回顾性分析2011年1月—2020年12月于中山大学附属第三医院住院的960例不明肝病行肝活检患者的病因,按照年份、年龄阶段进行分类,计数资料多组间比较采用χ2检验,非正态分布的计量资料多组间比较采用Kruskal-Wallis H检验。 结果 近10年不明原因肝病构成比总体呈上升趋势,肝活检后确诊疾病谱中第1位为自身免疫性肝病(AILD),共306例(31.9%);第2位为非酒精性脂肪性肝病(NAFLD),共95例(9.9%);第3位为药物性肝损伤(DILI),共82例(8.5%);病因不明者320例(33.3%)。各类病因的性别比、中位年龄分布均有统计学差异(χ2=155.36,P<0.001;H=182.48,P<0.001)。在2011—2020年已确诊的病因中,AILD一直居于首位,其构成比总体呈下降趋势(χ2=24.40,P<0.001)。在少年阶段中确诊最多为NAFLD(17.6%),青年、中年、老年阶段确诊最多均为AILD(17.8%、47.3%、56.3%)。 结论 近10年肝活检患者中不明原因肝病构成比呈上升趋势,其肝活检后诊断疾病谱以AILD为主,其次为NAFLD和DILI,但仍有1/3的患者病因诊断不明。 Abstract:Objective To investigate the composition ratios and trends of different etiologies after liver biopsy for patients with unexplained liver diseases. Methods A retrospective analysis was performed for the etiology of 960 patients with unexplained liver diseases who were hospitalized and underwent liver biopsy in The Third Affiliated Hospital of Sun Yat-Sen University from January 2011 to December 2020, and the etiologies were categorized by year and age group. The chi-square test was used for comparison of categorical data between multiple groups, and the Kruskal-Wallis H test was used for comparison of non-normally distributed continuous data between multiple groups. Results There was a tendency of increase in the overall composition ratio of unexplained liver diseases over the past decade. The leading diagnosis after liver biopsy was autoimmune liver disease (AILD) in 306 patients (31.9%), followed by nonalcoholic fatty liver disease (NAFLD) in 95 patients (9.9%) and drug-induced liver disease (DILI) in 82 patients (8.5%), and there were still 320 patients with undetermined causes (33.3%). There were significant differences in sex ratio and median age distribution between the patients with different etiologies (sex ratio: χ2=155.36, P<0.001; median age distribution: H=182.48, P<0.001). AILD had been the leading etiology in 2011 — 2020, and there was a tendency of reduction in the composition ratio of AILD (χ2=24.40, P<0.001). NAFLD accounted for the highest proportion of 17.6% in the adolescent stage, while AILD accounted for the highest proportion of 17.8%, 47.3%, and 56.3%, respectively, in the young, middle-aged, and elderly stages. Conclusion There is a tendency of increase in the composition ratio of unexplained liver diseases in patients undergoing liver biopsy, with AILD being the main disease diagnosed after liver biopsy, followed by NAFLD and DILI, but one-third of the patients still have an unclear etiological diagnosis. -
Key words:
- Liver Diseases /
- Biopsy /
- Spectrum of Disease
-
表 1 不明原因肝病行肝活检患者的一般资料
Table 1. General information of patients undergoing liver biopsy for unexplained liver disease
肝活检后病因 例数(%) 男/女(例) 年龄(岁) 病因不明 320(33.3) 196/124 37(5~78) AILD 306(31.9) 71/235 50(8~75) NAFLD 95(9.9) 76/19 33(11~56) DILI 82(8.5) 37/45 47(15~67) 遗传代谢性肝病 37(3.9) 26/11 24(13~62) 酒精性肝病 15(1.6) 13/2 47(28~59) 其他肝病 105(10.9) 60/45 40(21~66) 统计值 χ2=155.36 H=182.48 P值 <0.001 <0.001 -
[1] YANG YF. Road map of diagnosis in patients with unknown causes[J]. J Pract Hepatol, 2018, 21( 1): 1- 3. DOI: 10.3969/j.issn.1672-5069.2018.01.001.杨永峰. 不明原因肝病诊断思路[J]. 实用肝脏病杂志, 2018, 21( 1): 1- 3. DOI: 10.3969/j.issn.1672-5069.2018.01.001. [2] CHOWDHURY AB, MEHTA KJ. Liver biopsy for assessment of chronic liver diseases: A synopsis[J]. Clin Exp Med, 2023, 23( 2): 273- 285. DOI: 10.1007/s10238-022-00799-z. [3] CAMPBELL MS, REDDY KR. Review article: The evolving role of liver biopsy[J]. Aliment Pharmacol Ther, 2004, 20( 3): 249- 259. DOI: 10.1111/j.1365-2036.2004.02071.x. [4] Chinese Society of Hepatology and Chinese Society of Infectious Diseases, Chinese Medical Association. The guideline of prevention and treatment for chronic hepatitis B: a 2015 update[J]. J Clin Hepatol, 2015, 31( 12): 1941- 1960. DOI: 10.3969/j.issn.1001-5256.2015.12.002.中华医学会肝病学分会, 中华医学会感染病学分会. 慢性乙型肝炎防治指南(2015年更新版)[J]. 临床肝胆病杂志, 2015, 31( 12): 1941- 1960. DOI: 10.3969/j.issn.1001-5256.2015.12.002. [5] Chinese Society of Infectious Diseases, Chinese Medical Association; Chinese Society of Hepatology, Chinese Medical Association. Guidelines for the prevention and treatment of chronic hepatitis B(version 2019)[J]. J Clin Hepatol, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007.中华医学会感染病学分会, 中华医学会肝病学分会. 慢性乙型肝炎防治指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35( 12): 2648- 2669. DOI: 10.3969/j.issn.1001-5256.2019.12.007. [6] Chinese Society of Hepatology, Chinese Medical Association; Chinese Society of Infectious Diseases, Chinese Medical Association. The guideline of prevention and treatment for chronic hepatitis B: a 2022 update[J]. Infect Dis Info, 2023, 36( 1): 1- 17. DOI: 10.3969/j.issn.1007-8134.2023.01.01.中华医学会肝病学分会, 中华医学会感染病学分会. 慢性乙型肝炎防治指南(2022年版)[J]. 传染病信息, 2023, 36( 1): 1- 17. DOI: 10.3969/j.issn.1007-8134.2023.01.01. [7] TOH BH. Diagnostic autoantibodies for autoimmune liver diseases[J]. Clin Transl Immunology, 2017, 6( 5): e139. DOI: 10.1038/cti.2017.14. [8] LIM J, KIM HJ. Epidemiology of autoimmune liver disease in Korea: Evidence from a nationwide real-world database[J]. Orphanet J Rare Dis, 2024, 19( 1): 178. DOI: 10.1186/s13023-024-03086-0. [9] PUROHIT T, CAPPELL MS. Primary biliary cirrhosis: Pathophysiology, clinical presentation and therapy[J]. World J Hepatol, 2015, 7( 7): 926- 941. DOI: 10.4254/wjh.v7.i7.926. [10] INVERNIZZI F, CILLA M, TRAPANI S, et al. Gender and autoimmune liver diseases: Relevant aspects in clinical practice[J]. J Pers Med, 2022, 12( 6): 925. DOI: 10.3390/jpm12060925. [11] HAN SK, BAIK SK, KIM MY. Non-alcoholic fatty liver disease: Definition and subtypes[J]. Clin Mol Hepatol, 2023, 29( suppl): S5- S16. DOI: 10.3350/cmh.2022.0424. [12] GOLDNER D, LAVINE JE. Nonalcoholic fatty liver disease in children: Unique considerations and challenges[J]. Gastroenterology, 2020, 158( 7): 1967- 1983. e 1. DOI: 10.1053/j.gastro.2020.01.048. [13] SHAUNAK M, BYRNE CD, DAVIS N, et al. Non-alcoholic fatty liver disease and childhood obesity[J]. Arch Dis Child, 2021, 106( 1): 3- 8. DOI: 10.1136/archdischild-2019-318063. [14] MANN JP, VALENTI L, SCORLETTI E, et al. Nonalcoholic fatty liver disease in children[J]. Semin Liver Dis, 2018, 38( 1): 1- 13. DOI: 10.1055/s-0038-1627456. [15] FERRAIOLI G, MAIOCCHI L, RACITI MV, et al. Detection of liver steatosis with a novel ultrasound-based technique: A pilot study using MRI-derived proton density fat fraction as the gold standard[J]. Clin Transl Gastroenterol, 2019, 10( 10): e00081. DOI: 10.14309/ctg.0000000000000081. [16] SHEN T, LIU YX, SHANG J, et al. Incidence and etiology of drug-induced liver injury in Mainland China[J]. Gastroenterology, 2019, 156( 8): 2230- 2241. e 11. DOI: 10.1053/j.gastro.2019.02.002. [17] FISHER K, VUPPALANCHI R, SAXENA R. Drug-induced liver injury[J]. Arch Pathol Lab Med, 2015, 139( 7): 876- 887. DOI: 10.5858/arpa.2014-0214-RA. [18] WANG YY, XIE P. Risk factors of liver injury in patients with hepatitis B virus infection and pulmonary tuberculosis and predictive model construction[J/OL]. Chin J Exp Clin Infect Dis(Electron Edition), 2023, 17( 4): 267- 273. DOI: 10.3877/cma.j.issn.1674-1358.2023.04.008.王迎迎, 谢平. 乙型肝炎病毒感染合并肺结核患者发生肝损伤的危险因素及预测模型构建[J/OL]. 中华实验和临床感染病杂志(电子版), 2023, 17( 4): 267- 273. DOI: 10.3877/cma.j.issn.1674-1358.2023.04.008. [19] HE Y, LI BL, LI H. Analysis of influencing factors on drug-induced liver injury induced by anti-tuberculosis therapy in patients with newly treated pulmonary tuberculosis combined with hepatitis B virus infection[J]. J Changchun Univ Chin Med, 2024, 40( 4): 450- 454. DOI: 10.13463/j.cnki.cczyy.2024.04.023.贺毅, 李榜龙, 李慧. 初治肺结核合并乙型肝炎病毒感染患者抗结核治疗诱发药物性肝损伤的影响因素分析[J]. 长春中医药大学学报, 2024, 40( 4): 450- 454. DOI: 10.13463/j.cnki.cczyy.2024.04.023. [20] ETTEL M, GONZALEZ GA, GERA S, et al. Frequency and pathological characteristics of drug-induced liver injury in a tertiary medical center[J]. Hum Pathol, 2017, 68: 92- 98. DOI: 10.1016/j.humpath.2017.08.029. [21] KHALIFA A, ROCKEY DC. The utility of liver biopsy in 2020[J]. Curr Opin Gastroenterol, 2020, 36( 3): 184- 191. DOI: 10.1097/mog.0000000000000621. [22] CHOWDHURY AB, MEHTA KJ. Liver biopsy for assessment of chronic liver diseases: A synopsis[J]. Clin Exp Med, 2023, 23( 2): 273- 285. DOI: 10.1007/s10238-022-00799-z. [23] SCHNEIDER AL, KÖHLER H, RÖTHLISBERGER B, et al. Sodium taurocholate co-transporting polypeptide deficiency[J]. Clin Res Hepatol Gastroenterol, 2022, 46( 3): 101824. DOI: 10.1016/j.clinre.2021.101824. [24] LIU ZX, ZHAO WH, CAO CX, et al. Pituitary stalk interruption syndrome and liver cirrhosis associated with diabetes and an inactivating KCNJ11 gene mutation: A case report and literature review[J]. Front Endocrinol(Lausanne), 2023, 14: 1297146. DOI: 10.3389/fendo.2023.1297146. [25] LIBERAL R, GRANT CR. Cirrhosis and autoimmune liver disease: Current understanding[J]. World J Hepatol, 2016, 8( 28): 1157- 1168. DOI: 10.4254/wjh.v8.i28.1157. [26] ZHENG YF, ZHANG XL, WENG YH, et al. Etiological spectrum and clinical features of patients with unexplained liver disease manifesting as isolated jaundice: An analysis of 91 cases[J]. J Clin Hepatol, 2023, 39( 5): 1105- 1109. DOI: 10.3969/j.issn.1001-5256.2023.05.016.郑玉凤, 张胥磊, 翁宇航, 等. 91例以单纯性黄疸为表现的不明原因肝病患者病因谱及临床特征分析[J]. 临床肝胆病杂志, 2023, 39( 5): 1105- 1109. DOI: 10.3969/j.issn.1001-5256.2023.05.016. -



 PDF下载 ( 1168 KB)
PDF下载 ( 1168 KB)

 下载:
下载: