乙型肝炎肝硬化患者门静脉高压改善的组织学因素分析
DOI: 10.12449/JCH250815
Histological factors for improving portal hypertension in patients with chronic hepatitis B cirrhosis
-
摘要:
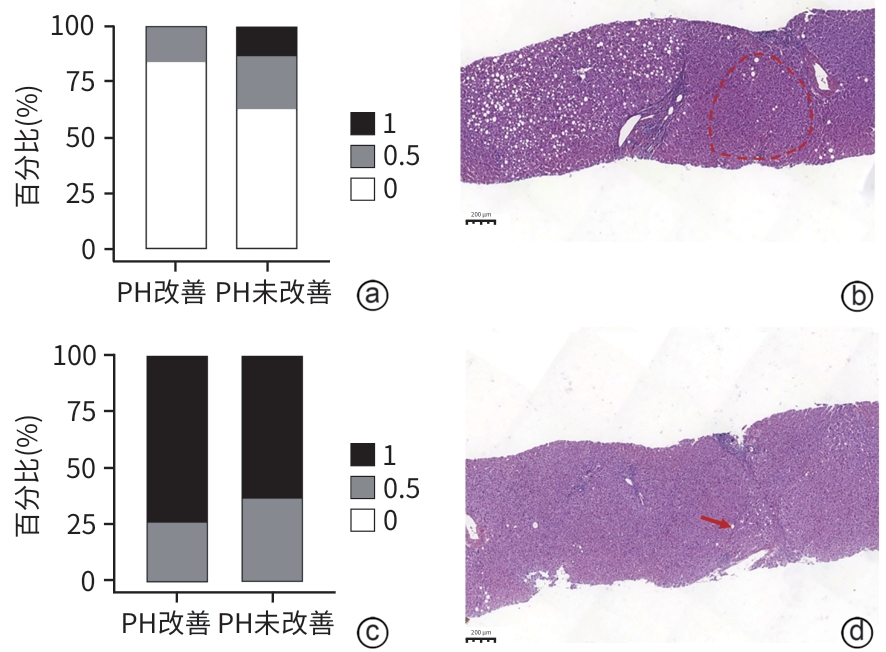
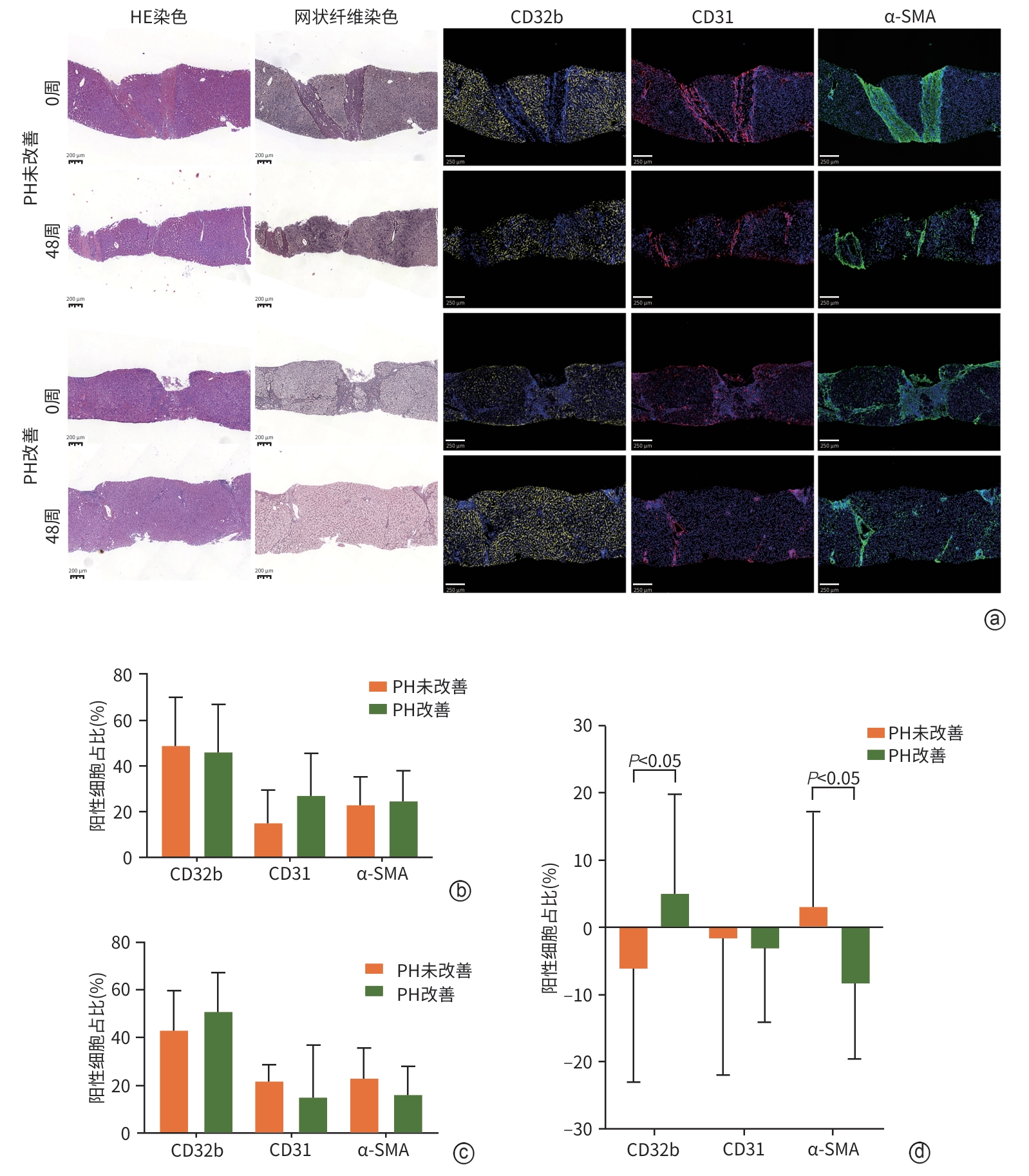
目的 通过观察肝硬化门静脉高压(PH)患者治疗前后的肝组织学变化,发现影响PH好转的组织学及细胞学基础,为临床药物研发提供依据。 方法 选取2014年9月—2018年10月在12个省20家医院招募的完成48周抗病毒或联合抗肝纤维化治疗的乙型肝炎肝硬化患者322例,使用Baveno Ⅶ中临床显著门静脉高压(CSPH)无创诊断标准评价PH水平,根据治疗前肝硬度值≥25 kPa筛选出43例确诊CSPH的患者,以治疗后PH水平下降是否≥2个等级分为PH改善组(n=19)及PH未改善组(n=24)。收集人口学、实验室检查资料,并进行肝纤维化评价(HE染色及网状纤维染色)和肝组织微血管病变评价[包括闭塞性门静脉病变(OPV)、结节性再生性增生(NRH)及不完全间隔纤维化(ISF)]。免疫组化检测血管性血友病因子(vWF)、纤维连接蛋白(Fibronectin)的表达水平;多重荧光免疫组化检测纤维蛋白原(Fibrinogen)、CD32b、CD31、α-平滑肌肌动蛋白(α-SMA)的表达水平。计量资料的两组间比较使用成组t检验或Mann-Whitney U检验,计数资料的两组间比较使用χ2检验。 结果 经过48周治疗,RBC、ALT、AST、APRI评分、肝纤维化等级与PH等级发生好转(P值均<0.05),其中19例患者PH等级下降≥2个等级,为PH改善组,其余为PH未改善组。两组患者间肝纤维化结局并无统计学差异(χ2=3.380,P=0.066)。微血管病变评价发现,治疗后PH改善组OPV程度、vWF表达水平及Fibronectin表达量显著低于PH未改善组(P值均<0.05),而NRH程度、ISF程度及Fibrinogen表达量无统计学差异(P值均>0.05)。细胞学评价发现,治疗前及治疗后两组间CD32b、CD31、α-SMA表达量无统计学意义(P值均>0.05),而治疗前后差值比较显示PH改善组CD32b表达量显著增加(t=-2.007,P=0.045),而α-SMA表达量显著减少(t=2.628,P=0.013)。 结论 PH改善的病理特征与肝纤维化逆转和肝微血管改善有关,其细胞学基础与肝窦内皮细胞去分化及肝星状细胞活化表型有关。 Abstract:Objective To investigate the histological and cellular bases for the improvement of portal hypertension (PH) by observing liver histopathological changes after treatment in patients with cirrhotic portal hypertension, and to provide a basis for clinical drug development. Methods A total of 322 patients with hepatitis B cirrhosis who completed 48 weeks of antiviral therapy or combined anti-fibrotic treatment in 20 hospitals across 12 provinces in China from September 2014 to October 2018 were enrolled, and the noninvasive diagnostic criteria for clinically significant portal hypertension (CSPH) from Baveno Ⅶ were used to assess the severity of PH; 43 patients with a confirmed diagnosis of CSPH were identified based on liver stiffness measurement (LSM) ≥25 kPa before treatment, and according to whether the severity of PH was reduced by ≥2 grades after treatment, the patients were divided into PH improvement (n=19) group and PH non-improvement group(n=24). Related data were collected, including demographic data, laboratory tests. Liver fibrosis were assessed, including HE staining and reticular fiber staining; liver microvascular lesions were assessed, including obliterative portal venopathy (OPV), nodular regenerative hyperplasia (NRH), and incomplete septal fibrosis (ISF). Single immunohistochemical staining was performed for von Willebrand factor (vWF), and fibronectin; multiplex immunohistochemical staining was performed for fibrinogen, CD32b, CD31, alpha-smooth muscle actin (α-SMA). The independent-samples t test or the Mann-Whitney U test was used for comparison of continuous data between two groups, and the chi-square test was used for comparison of categorical data between two groups. Results After 48 weeks of treatment, 43 patients had significant improvements in red blood cell count, alanine aminotransferase, aspartate aminotransferase, aspartate aminotransferase-to-platelet ratio index score, liver fibrosis grade, and PH grade (all P<0.05), among whom 19 patients showed a reduction in PH severity by ≥2 grades (PH improvement group), while the remaining patients were enrolled as the PH non-improvement group. There was no significant difference in the outcome of liver fibrosis between the two groups (χ²=3.380, P=0.066). Microvascular lesion assessment showed that compared with the PH non-improvement group, the PH improvement group had significantly lower OPV severity, microvascular density (the expression level of vWF), and expression of fibronectin (all P<0.05), while there were no significant differences in NRH severity, ISF severity, and the expression level of fibrinogen between the two groups (all P>0.05). Cytological evaluation showed no significant differences in the expression levels of CD32b, CD31, and α-SMA between the two groups before and after treatment (all P>0.05), and comparison of the expression levels before and after treatment showed that the PH improvement group had a significant increase in the expression level of CD32b (t=-2.007, P=0.045) and a significant reduction in the expression level of α-SMA (t=2.628, P=0.013). Conclusion The pathological features of PH improvement are associated with liver fibrosis regression and the improvement in liver microvascular lesions, and at the cellular level, PH improvement is associated with the dedifferentiation of liver sinusoidal endothelial cells and the activated phenotype of hepatic stellate cells. -
Key words:
- Hepatitis B /
- Liver Cirrhosis /
- Hypertension, Portal /
- Histology /
- Microvessels
-
表 1 Baveno Ⅶ共识的无创诊断CSPH标准
Table 1. Baveno Ⅶ criteria for noninvasive diagnosis of CSPH
PH等级 1 2 3 4 4 5 LSM(kPa) <5 <10 ≥10~15 ≥15~20 ≥20~25 ≥25 PLT(×109/L) 任何 任何 ≥150 <110 <150 任何 表 2 肝组织微血管病变评价标准
Table 2. Criteria for evaluating microangiopathy in liver tissue
评分 OPV NRH ISF 0分 0 0 0 0.5分 <25% <25% <25% 1.0分 25%~<50% 25%~<50% 25%~<50% 1.5分 50%~<75% 50%~<75% 50%~<75% 2.0分 ≥75% ≥75% ≥75% 注:%代表病变范围累及总汇管区数量的百分比。
表 3 43例患者治疗前后临床资料比较
Table 3. Comparison of clinical data for all patients before and after treatment
项目 0周 48周 统计值 P值 RBC(×1012/L) 4.50±0.55 4.82±0.47 t=-2.828 0.006 Hb(g/L) 141.54±18.19 146.64±18.10 t=-1.302 0.197 WBC(×109/L) 4.68±1.41 4.96±1.26 t=-1.001 0.320 PLT(×109/L) 99.00(65.00~121.00) 111.00(65.00~131.00) Z=-1.607 0.054 ALT(U/L) 52.00(30.00~73.40) 37.00(28.00~57.00) Z=-1.862 0.031 AST(U/L) 47.00(33.00~67.00) 37.00(29.00~47.00) Z=-2.540 0.011 TBil(μmol/L) 14.90(11.60~21.40) 16.30(12.50~21.60) Z=-0.428 0.672 Alb(g/L) 41.34±6.15 40.93±6.12 t=-0.310 0.757 PT(s) 13.95±1.64 13.43±1.46 t=1.324 0.189 Cr(mmol/L) 70.33±15.68 71.02±16.17 t=-0.203 0.840 LSM(kPa) 27.30(25.60~35.30) 15.70(11.10~18.90) Z=-7.368 <0.001 FIB-4评分(分) 3.70(2.65~5.87) 2.56(1.84~3.75) Z=-1.689 0.092 APRI评分(分) 1.31(0.90~2.01) 1.00(0.64~1.36) Z=-2.669 0.007 Ishak评分[例(%)] χ2=-2.969 0.003 6分 18(41.67) 12(27.91) 5分 25(58.33) 16(37.21) 4分 0(0.00) 10(23.26) 3分 0(0.00) 4(9.30) 2分 0(0.00) 1(2.33) PH等级[例(%)] χ2=-6.270 <0.001 5 43(100.00) 15(34.88) 4 0(0.00) 9(20.93) 3 0(0.00) 14(32.56) 2 0(0.00) 5(11.63) 1 0(0.00) 0(0.00) 注:PT,凝血酶原时间;Cr,肌酐。
表 4 两组患者基线临床资料比较
Table 4. Comparison of baseline clinical data between the two groups
项目 PH未改善组(n=24) PH改善组(n=19) 统计值 P值 年龄(岁) 44.78±9.67 42.88±8.62 t=0.687 0.496 男/女(例) 23/1 12/7 χ2=7.477 0.006 BMI(kg/m2) 24.48±2.6 24.87±3.03 t=-0.451 0.654 RBC(×1012/L) 4.54±0.45 4.47±0.47 t=0.406 0.687 Hb(g/L) 145.77±12.39 136.21±22.85 t=1.642 0.113 WBC(×109/L) 4.68±1.47 4.67±1.37 t=0.035 0.972 PLT(×109/L) 88.25±29.35 101.84±31.13 t=-1.468 0.150 ALT(U/L) 55.00(31.25~84.00) 44.00(26.00~58.00) Z=-1.725 0.084 AST(U/L) 55.33±25.66 46.46±17.50 t=1.267 0.212 TBil(μmol/L) 19.38(12.28~22.75) 13.10(10.20~16.90) Z=-2.055 0.040 Alb(g/L) 41.68±6.29 40.93±6.12 t=0.392 0.697 PT(s) 14.36±1.69 13.43±1.46 t=1.893 0.065 Cr(mmol/L) 75.25±14.31 64.11±15.47 t=2.448 0.019 FIB-4评分(分) 3.70(2.65~5.87) 3.23(1.71~4.85) Z=-1.052 0.293 APRI评分(分) 1.73±0.90 1.31±0.76 t=1.627 0.111 Ishak评分 χ2=-0.052 0.977 6分 10(41.67) 8(42.11) 5分 14(58.33) 11(57.89) -
[1] BOSCH J, GROSZMANN RJ, SHAH VH. Evolution in the understanding of the pathophysiological basis of portal hypertension: How changes in paradigm are leading to successful new treatments[J]. J Hepatol, 2015, 62( 1 Suppl): S121- S130. DOI: 10.1016/j.jhep.2015.01.003. [2] GUIXÉ-MUNTET S, QUESADA-VÁZQUEZ S, GRACIA-SANCHO J. Pathophysiology and therapeutic options for cirrhotic portal hypertension[J]. Lancet Gastroenterol Hepatol, 2024, 9( 7): 646- 663. DOI: 10.1016/S2468-1253(23)00438-7. [3] GUO YN, LYU J, LIU CH. Medicinal treatment of portal hypertension in liver cirrhosis[J]. Chin J Integr Tradit West Med Liver Dis, 2021, 31( 11): 961- 964.郭亚楠, 吕靖, 刘成海. 肝硬化门静脉高压症的药物治疗[J]. 中西医结合肝病杂志, 2021, 31( 11): 961- 964. [4] SUN X, LIU CH. Consensus interpretation of Baveno Ⅶ in the diagnosis and treatment of portal hypertension in cirrhosis: A physician’s perspective[J]. Chin J Integr Tradit West Med Dig, 2023, 31( 2): 79- 84.孙鑫, 刘成海. 肝硬化门静脉高压诊治Baveno Ⅶ共识解读: 内科视角[J]. 中国中西医结合消化杂志, 2023, 31( 2): 79- 84. [5] de FRANCHIS R, BOSCH J, GARCIA-TSAO G, et al. Baveno VII-Renewing consensus in portal hypertension[J]. J Hepatol, 2022, 76( 4): 959- 974. DOI: 10.1016/j.jhep.2021.12.022. [6] CAMPRECIÓS G, VILASECA M, TRIPATHI DM, et al. Interspecies transcriptomic comparison identifies a potential Porto-sinusoidal vascular disorder rat model suitable for in vivo drug testing[J]. Liver Int, 2024, 44( 1): 180- 190. DOI: 10.1111/liv.15765. [7] WEIDNER N, SEMPLE JP, WELCH WR, et al. Tumor angiogenesis and metastasis: Correlation in invasive breast carcinoma[J]. N Engl J Med, 1991, 324( 1): 1- 8. DOI: 10.1056/NEJM199101033240101. [8] SELICEAN S, WANG C, GUIXÉ-MUNTET S, et al. Regression of portal hypertension: Underlying mechanisms and therapeutic strategies[J]. Hepatol Int, 2021, 15( 1): 36- 50. DOI: 10.1007/s12072-021-10135-4. [9] ABBEY P, SHALIMAR. Nodular regenerative hyperplasia[J]. Curr Hepatol Rep, 2023, 22( 3): 182- 192. DOI: 10.1007/s11901-023-00613-8. [0] WANLESS IR, NAKASHIMA E, SHERMAN M. Regression of human cirrhosis. Morphologic features and the genesis of incomplete septal cirrhosis[J]. Arch Pathol Lab Med, 2000, 124( 11): 1599- 1607. DOI: 10.5858/2000-124-1599-ROHC. [11] GRACIA-SANCHO J, MARRONE G, FERNÁNDEZ-IGLESIAS A. Hepatic microcirculation and mechanisms of portal hypertension[J]. Nat Rev Gastroenterol Hepatol, 2019, 16( 4): 221- 234. DOI: 10.1038/s41575-018-0097-3. [12] Chinese Society of Hepatology, Chinese Society of Gastroenterology, and Chinese Society of Digestive Endoscopology of Chinese Medical Association. Guidelines on the management of esophagogastric variceal bleeding in cirrhotic portal hypertension[J]. J Clin Hepatol, 2023, 39( 3): 527- 538. DOI: 10.3969/j.issn.1001-5256.2023.03.znygf.中华医学会肝病学分会, 中华医学会消化病学分会, 中华医学会消化内镜学分会. 肝硬化门静脉高压食管胃静脉曲张出血的防治指南[J]. 临床肝胆病杂志, 2023, 39( 3): 527- 538. DOI: 10.3969/j.issn.1001-5256.2023.03.znygf. [13] Beijing Society of Portal Hypertension, Beijing Medical Association; Portal Hypertension Expert Committee, Liver Disease Committee of Chinese Research Hospital Association; Liver Disease Committee of Chinese Research Hospital Association. Expert consensus on multidisciplinary diagnosis and treatment of cirrhotic portal hypertension(based on hepatic venous pressure gradient)[J]. J Clin Hepatol, 2021, 37( 9): 2037- 2044. DOI: 10.3969/j.issn.1001-5256.2021.09.008.北京医师协会门静脉高压专科医师分会, 中国研究型医院学会肝病专业委员会门静脉高压学组, 中国研究型医院学会肝病专业委员会. 肝硬化门静脉高压症多学科诊治(基于肝静脉压力梯度)专家共识[J]. 临床肝胆病杂志, 2021, 37( 9): 2037- 2044. DOI: 10.3969/j.issn.1001-5256.2021.09.008. [14] GRACIA-SANCHO J, MAESO-DÍAZ R, FERNÁNDEZ-IGLESIAS A, et al. New cellular and molecular targets for the treatment of portal hypertension[J]. Hepatol Int, 2015, 9( 2): 183- 191. DOI: 10.1007/s12072-015-9613-5. [15] GARCIA-TSAO G, FRIEDMAN S, IREDALE J, et al. Now there are many(stages) where before there was one: In search of a pathophysiological classification of cirrhosis[J]. Hepatology, 2010, 51( 4): 1445- 1449. DOI: 10.1002/hep.23478. [16] DAI WM, LU LG, CAI XB. Association between liver sinusoidal endothelial cells and liver fibrosis[J]. J Clin Hepatol, 2023, 39( 2): 419- 423. DOI: 10.3969/j.issn.1001-5256.2023.02.027.戴伟明, 陆伦根, 蔡晓波. 肝窦内皮细胞与肝纤维化的关系[J]. 临床肝胆病杂志, 2023, 39( 2): 419- 423. DOI: 10.3969/j.issn.1001-5256.2023.02.027. [17] LI MB, LI JY, FENG DP. Research advances in the reversal of liver fibrosis[J]. J Clin Hepatol, 2023, 39( 1): 193- 198. DOI: 10.3969/j.issn.1001-5256.2023.01.030.李满彪, 李金玉, 冯对平. 肝纤维化逆转的研究进展[J]. 临床肝胆病杂志, 2023, 39( 1): 193- 198. DOI: 10.3969/j.issn.1001-5256.2023.01.030. [18] IWAKIRI Y, TREBICKA J. Portal hypertension in cirrhosis: Pathophysiological mechanisms and therapy[J]. JHEP Rep, 2021, 3( 4): 100316. DOI: 10.1016/j.jhepr.2021.100316. [19] NAKASHIMA E, KAGE M, WANLESS IR. Idiopathic portal hypertension: histologic evidence that some cases may be regressed cirrhosis with portal vein thrombosis[J]. Hepatology, 1999, 30: 218A. [20] GUIDO M, SARCOGNATO S, RUSSO FP, et al. Focus on histological abnormalities of intrahepatic vasculature in chronic viral hepatitis[J]. Liver Int, 2018, 38( 10): 1770- 1776. DOI: 10.1111/liv.13718. [21] FERNANDEZ M. Molecular pathophysiology of portal hypertension[J]. Hepatology, 2015, 61( 4): 1406- 1415. DOI: 10.1002/hep.27343. -



 PDF下载 ( 3211 KB)
PDF下载 ( 3211 KB)


 下载:
下载: