甘油三酯葡萄糖指数联合C反应蛋白对新发非酒精性脂肪性肝病的影响
DOI: 10.12449/JCH250812
Effect of triglyceride-glucose index combined with C-reactive protein on new-onset nonalcoholic fatty liver disease
-
摘要:
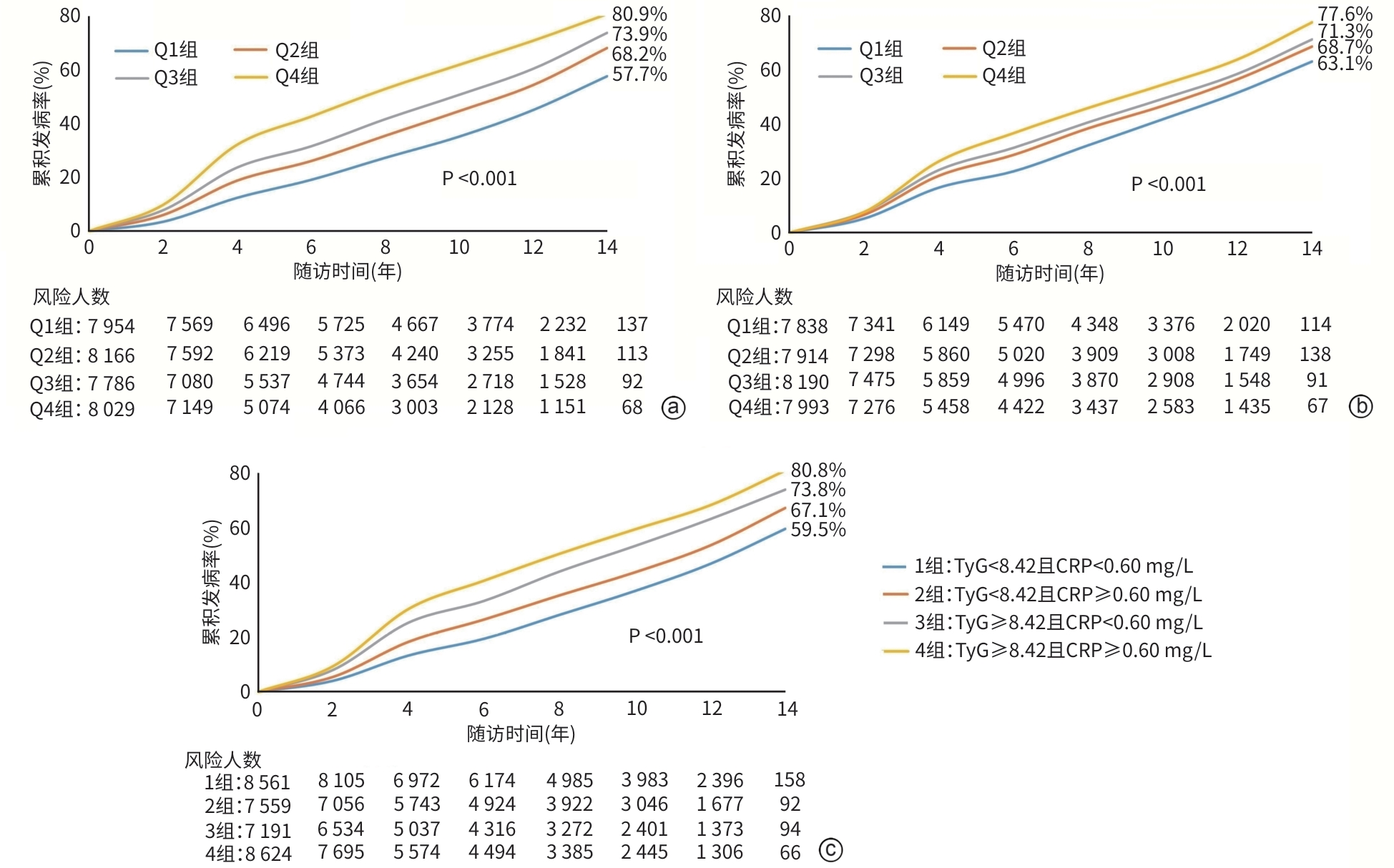
目的 通过观察甘油三酯葡萄糖指数(TyG)与C反应蛋白(CRP)不同水平组合对新发非酒精性脂肪性肝病(NAFLD)的影响,了解二者对NAFLD有无协同致病效应,为筛查NAFLD高风险人群提供依据。 方法 以参加2006—2007年健康体检、既往无饮酒史、无脂肪肝、无心血管疾病、无恶性肿瘤且未服用降糖、降脂药物的31 935例开滦集团公司职工为观察队列。根据基线CRP和TyG的中位数将研究对象分为4组,即TyG<8.42且CRP<0.60 mg/L组、TyG<8.42且CRP≥0.60 mg/L组、TyG≥8.42且CRP<0.60 mg/L组和TyG≥8.42且CRP≥0.60 mg/L组。正态分布的计量资料多组间比较采单因素方差分析。偏态分布计量资料,经对数转换后用方差分析进行组间比较。计数资料组间比较应用χ2检验。采用Kaplan-Meier法计算CRP与TyG不同水平组合的NAFLD累积发病率。采用多因素Cox回归模型分析TyG与CRP的不同水平组合对NAFLD发病的影响。 结果 在平均随访7.59年后,共有16 592例员工发生NAFLD。TyG<8.42且CRP<0.60 mg/L组、TyG<8.42且CRP≥0.60 mg/L组、TyG≥8.42且CRP<0.60 mg/L组和TyG≥8.42且CRP≥0.60 mg/L组的NAFLD累积发病率分别为59.5%、67.1%、73.8%和80.8%(P<0.001)。在校正混杂因素后,与TyG<8.42且CRP<0.60 mg/L组相比,TyG≥8.42且CRP≥0.60 mg/L组发生NAFLD的风险最高(HR=1.54,95%CI:1.47~1.61),其次为TyG≥8.42且CRP<0.60 mg/L组(HR=1.43,95%CI:1.36~1.49)和TyG<8.42且CRP≥0.60 mg/L组(HR=1.17,95%CI:1.12~1.22)。 结论 随着TyG和CRP水平升高,NAFLD累积发病率上升,二者水平的升高显著增加NAFLD的发病风险。 Abstract:Objective To investigate whether there is a synergistic pathogenic effect between triglyceride glucose index (TyG) and C-reactive protein (CRP) on new-onset nonalcoholic fatty liver disease (NAFLD) by observing the influence of combinations of TyG and CRP at different levels, and to provide a basis for identifying the high-risk population of NAFLD. Methods A total of 31 935 employees in Kailuan Group who participated in physical examination in 2006 — 2007 were enrolled as the observation cohort, and they had no history of drinking, fatty liver disease, cardiovascular disease, or malignant tumor and did not take antidiabetic or lipid-lowering drugs. According to the median of TyG and CRP at baseline, the subjects were divided into TyG<8.42 and CRP<0.60 mg/L group, TyG<8.42 and CRP≥0.60 mg/L group, TyG≥8.42 and CRP<0.60 mg/L group, and TyG≥8.42 and CRP≥0.60 mg/L group. A one-way analysis of variance was used for comparison of normally distributed continuous data between multiple groups, and an analysis of variance was used for comparison of continuous data with skewed distribution between groups after logarithmic transformation; the chi-square test was used for comparison of categorical data between groups. The Kaplan-Meier method was used to calculate the cumulative incidence rate of NAFLD in different combinations of CRP and TyG levels, and the multivariate Cox regression model was used to investigate the influence of different combinations of TyG and CRP on the incidence rate of NAFLD. Results After a mean follow-up time of 7.59 years, a total of 16 592 employees developed NAFLD. The cumulative incidence rate of NAFLD in the TyG<8.42 and CRP<0.60 mg/L group, TyG<8.42 and CRP≥0.60 mg/L group, TyG≥8.42 and CRP<0.60 mg/L group, and TyG≥8.42 and CRP≥0.60 mg/L group were 59.5%, 67.1%, 73.8%, and 80.8%, respectively (P<0.001). After adjustment for confounding factors, compared with the TyG<8.42 and CRP<0.60 mg/L group, the TyG≥8.42 and CRP≥0.60 mg/L group had the highest risk of developing NAFLD (hazard ratio [HR]=1.54, 95% confidence interval [CI]: 1.47 — 1.61), followed by the TyG≥8.42 and CRP<0.60 mg/L group (HR=1.43, 95%CI: 1.36 — 1.49) and the TyG<8.42 and CRP≥0.60 mg/L group (HR=1.17, 95%CI: 1.12 — 1.22). Conclusion With elevated TyG and CRP levels, the cumulative incidence of NAFLD increased, and rising levels of these markers significantly augmented the risk of NAFLD development. -
Key words:
- Non-alcoholic Fatty Liver Disease /
- C-Reactive Protein /
- Risk Factors
-
表 1 不同TyG与CRP水平组合人群的基线特征
Table 1. Baseline characteristics of different combinations of TyG and CRP levels
变量 TyG<8.42且
CRP<0.60 mg/L组
(n=8 561)TyG<8.42且
CRP≥0.60 mg/L组
(n=7 559)TyG≥8.42且
CRP<0.60 mg/L组
(n=7 191)TyG≥8.42且
CRP≥0.60 mg/L组
(n=8 624)统计值 P值 年龄(岁) 47.8±12.0 50.6±13.1 50.0±10.9 52.6±11.7 F=236.0 <0.001 男[例(%)] 4 887(57.1) 4 563(60.4) 5 178(72.0) 5 994(69.5) χ2=533.7 <0.001 SBP(mmHg) 121.9±18.3 124.8±20.3 128.4±19.2 131.3±20.2 F=373.1 <0.001 DBP(mmHg) 78.8±10.6 79.8±11.0 82.6±11.0 83.6±11.3 F=350.4 <0.001 腰围(cm) 81.4±10.2 82.9±9.7 84.9±9.3 86.8±9.5 F=478.4 <0.001 BMI(kg/m2) 22.9±2.9 23.7±3.1 24.2±2.9 24.9±3.0 F=693.2 <0.001 吸烟[例(%)] 996(11.6) 1 036(13.7) 888(12.3) 1 082(12.5) χ2=16.1 0.001 平均收入≥1 000元/月[例(%)] 858(10.0) 855(11.3) 523(7.3) 753(8.7) χ2=79.6 <0.001 体育锻炼[例(%)] 8 084(94.4) 7 125(94.3) 6 845(95.2) 8 220(95.3) χ2=14.8 0.002 高中及以上文化水平[例(%)] 1 563(18.3) 1 588(21.0) 781(10.9) 1 079(12.5) χ2=397.9 <0.001 ALT(U/L) 15.0(11.0~20.8) 15.0(11.0~21.0) 18.0(13.0~23.0) 18.0(13.0~23.0) F=192.3 <0.001 TC(mmol/L) 4.68±0.89 4.72±0.90 4.95±1.23 5.07±1.14 F=269.1 <0.001 LDL-C(mmol/L) 2.21±0.73 2.18±0.97 2.36±0.74 2.32±0.94 F=78.3 <0.001 TG(mmol/L) 0.80(0.63~0.98) 0.84(0.66~1.01) 1.53(1.27~2.07) 1.59(1.29~2.17) F=11 772.7 <0.001 HDL-C(mmol/L) 1.56±0.39 1.56±0.39 1.57±0.40 1.56±0.39 F=0.9 0.402 FBG(mmol/L) 4.86±0.61 4.84±0.68 5.50±1.58 5.62±1.73 F=869.1 <0.001 SUA(μmol/L) 247.2±65.7 258.2±71.1 265.3±69.7 275.5±76.0 F=240.6 <0.001 CRP(mg/L) 0.20(0.10~0.33) 1.50(0.90~3.20) 0.23(0.11~0.38) 1.50(0.90~3.06) F=18 373.2 <0.001 TyG 7.99±0.31 8.03±0.31 8.90±0.45 8.94±0.47 F=14 368.3 <0.001 eGFR(mL·min-1·1.73 m-2) 74.6±26.2 74.4±25.9 68.4±22.3 69.1±24.8 F=142.8 <0.001 注:SBP,收缩压;DBP,舒张压;FBG,空腹血糖;SUA,血尿酸;eGFR,估算的肾小球滤过率。
表 2 不同CRP亚组的TyG水平对新发NAFLD影响的Cox回归分析
Table 2. Cox regression analysis of the effects of TyG levels in different CRP subgroups on new-onset NAFLD
指标 TyG每增加1单位 TyG四分位组 P trend Q1组 Q2组 Q3组 Q4组 总人群 病例数/总人数 3 233/7 954 3 995/8 166 4 222/7 786 5 142/8 029 发病密度(/千人年) 47.3 62.0 73.6 98.4 HR(95%CI) 1.35(1.32~1.38) 1.00 1.21(1.16~1.27) 1.38(1.32~1.45) 1.69(1.61~1.77) <0.001 CRP<0.60 mg/L 病例数/总人数 1 679/4 453 1 932/4 108 1 925/3 699 2 161/3 492 发病密度(/千人年) 42.4 57.4 68.0 90.2 HR(95%CI) 1.39(1.34~1.44) 1.00 1.22(1.15~1.31) 1.40(1.31~1.50) 1.75(1.63~1.87) <0.001 CRP≥0.60 mg/L 病例数/总人数 1 554/3 501 2 063/4 058 2 297/4 087 2 981/4 537 发病密度(/千人年) 53.9 67.0 79.1 105 HR(95%CI) 1.31(1.27~1.36) 1.00 1.19(1.11~1.27) 1.33(1.25~1.43) 1.62(1.51~1.72) <0.001 注:CRP亚组与TyG四分位组的交互P=0.208。
表 3 不同TyG亚组的CRP水平对新发NAFLD影响的Cox回归分析
Table 3. Cox regression analysis of the effects of CRP levels in different TyG subgroups on new-onset NAFLD
指标 CRP每增加1 mg/L CRP四分位组 P trend Q1组 Q2组 Q3组 Q4组 总人群 病例数/总人数 3 656/7 838 4 041/7 914 4 294/8 190 4 601/7 993 发病密度(/千人年) 56.5 66.4 70.8 81.6 HR(95%CI) 1.04(1.03~1.04) 1.00 1.10(1.05~1.15) 1.11(1.06~1.16) 1.27(1.22~1.33) <0.001 TyG<8.42 病例数/总人数 1 820/4 513 1 791/4 048 1 700/3 812 1 917/3 747 发病密度(/千人年) 45.8 53.4 55.6 66.0 HR(95%CI) 1.04(1.03~1.06) 1.00 1.10(1.03~1.18) 1.12(1.05~1.20) 1.33(1.24~1.42) <0.001 TyG≥8.42 病例数/总人数 1 836/3 325 2 250/3 866 2 594/4 378 2 684/4 246 发病密度(/千人年) 73.5 82.4 86.4 98.3 HR(95%CI) 1.03(1.02~1.04) 1.00 1.08(1.02~1.15) 1.07(1.00~1.14) 1.19(1.12~1.27) <0.001 注:TyG亚组与CRP四分位组的交互P=0.509。
表 4 不同TyG与CRP水平组合对新发NAFLD影响的Cox回归分析
Table 4. Cox regression analysis of the effects of different combinations of TyG and CRP levels on new-onset NAFLD
指标 TyG<8.42且
CRP<0.60 mg/L组TyG<8.42且
CRP≥0.60 mg/L组TyG≥8.42且
CRP<0.60 mg/L组TyG≥8.42且
CRP≥0.60 mg/L组P trend 病例数/总人数 3 611/8 561 3 617/7 559 4 086/7 191 5 278/8 624 发病密度(/千人年) 49.3 60.7 78.2 92.0 HR(95%CI)1) 1.00 1.17(1.12~1.22) 1.43(1.36~1.49) 1.54(1.47~1.61) <0.001 HR(95%CI)1)2) 1.00 1.25(1.18~1.32) 1.48(1.39~1.57) 1.68(1.59~1.78) <0.001 注:1)校正年龄、性别、文化程度、体育锻炼、收入水平、吸烟、SBP、BMI、LDL-C、HDL-C、SUA、ALT和eGFR; 2)排除随访期间饮酒者(n=11 181)以及随访期间发生心肌梗死(n=101)、脑卒中(n=360)、恶性肿瘤者(n=328)、服用降脂(n=161)、降糖药物(n=429)者。
-
[1] YOUNOSSI ZM, KOENIG AB, ABDELATIF D, et al. Global epidemiology of nonalcoholic fatty liver disease: Meta-analytic assessment of prevalence, incidence, and outcomes[J]. Hepatology, 2016, 64( 1): 73- 84. DOI: 10.1002/hep.28431. [2] BYRNE CD, TARGHER G. Non-alcoholic fatty liver disease-related risk of cardiovascular disease and other cardiac complications[J]. Diabetes Obes Metab, 2022, 24( Suppl 2): 28- 43. DOI: 10.1111/dom.14484. [3] MUSSO G, GAMBINO R, TABIBIAN JH, et al. Association of non-alcoholic fatty liver disease with chronic kidney disease: A systematic review and meta-analysis[J]. PLoS Med, 2014, 11( 7): e1001680. DOI: 10.1371/journal.pmed.1001680. [4] MANTOVANI A, PETRACCA G, BEATRICE G, et al. Non-alcoholic fatty liver disease and increased risk of incident extrahepatic cancers: A meta-analysis of observational cohort studies[J]. Gut, 2022, 71( 4): 778- 788. DOI: 10.1136/gutjnl-2021-324191. [5] LI F, LI MW, WANG YS. Therapeutic paradigms and potential therapies for nonalcoholic steatohepatitis[J]. J Clin Hepatol, 2024, 40( 10): 2082- 2086. DOI: 10.12449/JCH241025.李凤, 李茂微, 王雨杉. 非酒精性脂肪肝病的治疗模式和潜在疗法[J]. 临床肝胆病杂志, 2024, 40( 10): 2082- 2086. DOI: 10.12449/JCH241025. [6] LI L, LIU DW, YAN HY, et al. Obesity is an independent risk factor for non-alcoholic fatty liver disease: Evidence from a meta-analysis of 21 cohort studies[J]. Obes Rev, 2016, 17( 6): 510- 519. DOI: 10.1111/obr.12407. [7] VACHLIOTIS I, GOULAS A, PAPAIOANNIDOU P, et al. Nonalcoholic fatty liver disease: Lifestyle and quality of life[J]. Hormones(Athens), 2022, 21( 1): 41- 49. DOI: 10.1007/s42000-021-00339-6. [8] MARJOT T, MOOLLA A, COBBOLD JF, et al. Nonalcoholic fatty liver disease in adults: Current concepts in etiology, outcomes, and management[J]. Endocr Rev, 2020, 41( 1): bnz009. DOI: 10.1210/endrev/bnz009. [9] ZHU F, WANG LM, JI CP, et al. Relationship between the C-reactive protein and nonalcoholic fatty liver disease prevalence[J]. Clin Med China, 2015, 31( 9): 812- 816. DOI: 10.3760/cma.j.issn.1008- 6315.2015.09.013.朱峰, 王来明, 季春鹏, 等. 血清C反应蛋白与非酒精性脂肪性肝病的相关性研究[J]. 中国综合临床, 2015, 31( 9): 812- 816. DOI: 10.3760/cma.j.issn.1008- 6315.2015.09.013. [10] ZHU F, WANG LM, JI CP, et al. Predictive value of C-reactive protein in emerging non-alcoholic fatty liver disease[J]. Chin J Hepatol, 2016, 24( 8): 575- 579. DOI: 10.3760/cma.j.issn.1007-3418. 2016.08.004.朱峰, 王来明, 季春鹏, 等. C-反应蛋白对新发非酒精性脂肪肝的预测价值[J]. 中华肝脏病杂志, 2016, 24( 8): 575- 579. DOI: 10.3760/cma.j.issn.1007-3418.2016.08.004. [11] CHEN CX, DU J, SONG J, et al. Study on correlation between serum hypersensitive C-reactive protein and nonalcoholic fatty liver disease in the elderly[J]. Chin J Gen Prac, 2023, 21( 9): 1491- 1494. DOI: 10.16766/j.cnki.issn.1674-4152.003153.陈长喜, 杜娟, 宋健, 等. 血清超敏C反应蛋白与老年人非酒精性脂肪肝的相关性[J]. 中华全科医学, 2023, 21( 9): 1491- 1494. DOI: 10.16766/j.cnki.issn.1674-4152.003153. [12] LING Q, CHEN JW, LIU X, et al. The triglyceride and glucose index and risk of nonalcoholic fatty liver disease: A dose-response meta-analysis[J]. Front Endocrinol(Lausanne), 2023, 13: 1043169. DOI: 10.3389/fendo.2022.1043169. [13] National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update[J]. J Clin Hepatol, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007.中华医学会肝病学分会脂肪肝和酒精性肝病学组, 中国医师协会脂肪性肝病专家委员会. 非酒精性脂肪性肝病防治指南(2018年更新版)[J]. 临床肝胆病杂志, 2018, 34( 5): 947- 957. DOI: 10.3969/j.issn.1001-5256.2018.05.007. [14] ZHENG RJ, DU ZN, WANG MM, et al. A longitudinal epidemiological study on the triglyceride and glucose index and the incident nonalcoholic fatty liver disease[J]. Lipids Health Dis, 2018, 17( 1): 262. DOI: 10.1186/s12944-018-0913-3. [15] KIM KS, HONG SM, AHN HY, et al. Triglyceride and glucose index is a simple and easy-to-calculate marker associated with nonalcoholic fatty liver disease[J]. Obesity(Silver Spring), 2022, 30( 6): 1279- 1288. DOI: 10.1002/oby.23438. [16] LEE J, YOON K, RYU S, et al. High-normal levels of hs-CRP predict the development of non-alcoholic fatty liver in healthy men[J]. PLoS One, 2017, 12( 2): e0172666. DOI: 10.1371/journal.pone.0172666. [17] ZHANG YX, WANG Y, YOU CL, et al. Analysis of related factors of abnormal liver function in patients with nonalcoholic fatty liver disease[J]. Clin J Med Offic, 2025, 53( 5): 522- 524,528. DOI: 10.16680/j.1671-3826.2025.05.21.张月霞, 王宇, 尤丛蕾, 等. 非酒精性脂肪肝患者肝功能异常相关因素分析[J]. 临床军医杂志, 2025, 53( 5): 522- 524, 528. DOI: 10.16680/j.1671-3826.2025.05.21. [18] LEE JW, CHO YK, RYAN M, et al. Serum uric Acid as a predictor for the development of nonalcoholic fatty liver disease in apparently healthy subjects: A 5-year retrospective cohort study[J]. Gut Liver, 2010, 4( 3): 378- 383. DOI: 10.5009/gnl.2010.4.3.378. [19] KIDA Y, SATO T. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease[J]. Ann Intern Med, 2006, 144( 5): 379- 380; author reply 380. DOI: 10.7326/0003-4819-144-5-200603070-00022. [20] MIN YY, ZHANG P, TIAN PR, et al. The mechanism of bariatric surgery in the treatment of non-alcoholic fatty liver disease[J]. Chin J Dig Surg, 2024, 23( 9): 1231- 1236. DOI: 10.3760/cma.j.cn115610-20240614-00296.闵逸洋, 张鹏, 田沛荣, 等. 减重手术治疗非酒精性脂肪性肝病的作用机制[J]. 中华消化外科杂志, 2024, 23( 9): 1231- 1236. DOI: 10.3760/cma.j.cn115610-20240614-00296. [21] GRANDER C, GRABHERR F, TILG H. Non-alcoholic fatty liver disease: Pathophysiological concepts and treatment options[J]. Cardiovasc Res, 2023, 119( 9): 1787- 1798. DOI: 10.1093/cvr/cvad095. -



 PDF下载 ( 1033 KB)
PDF下载 ( 1033 KB)

 下载:
下载:


