甘油三酯-葡萄糖(TyG)指数与女性胆囊结石的相关性分析
DOI: 10.12449/JCH250727
Association between triglyceride-glucose index and gallstones in women: A cross-sectional study
-
摘要:
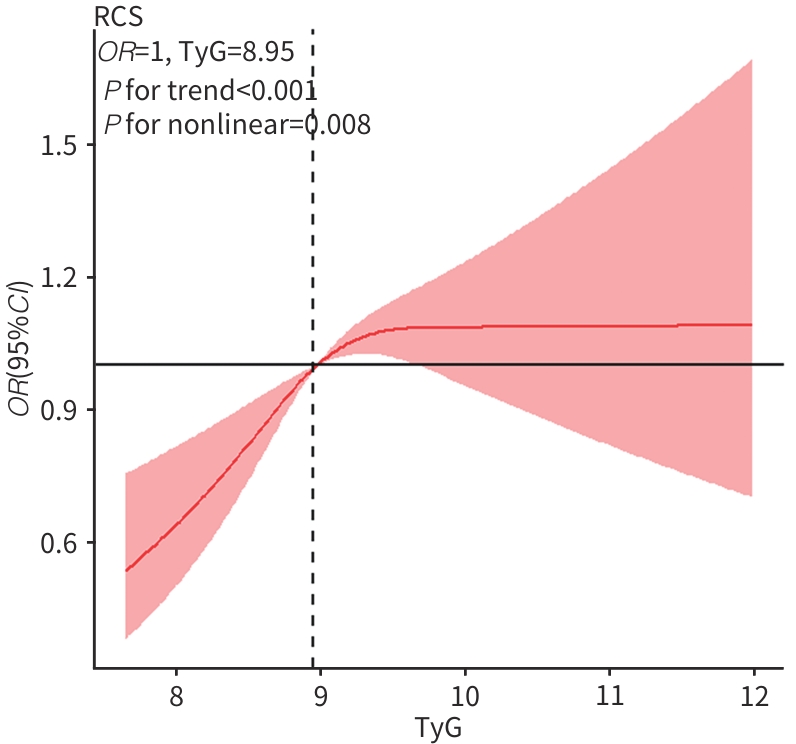
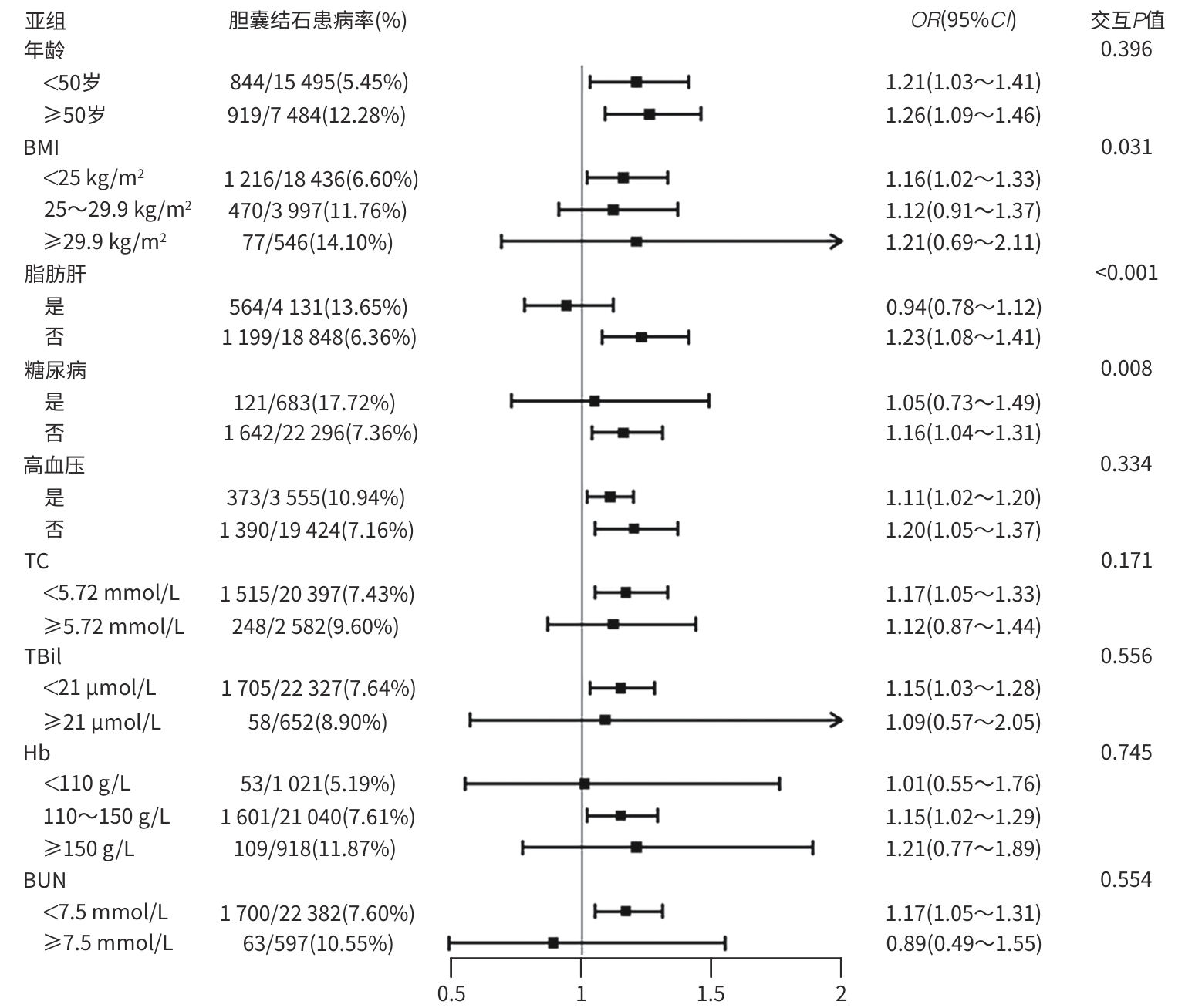
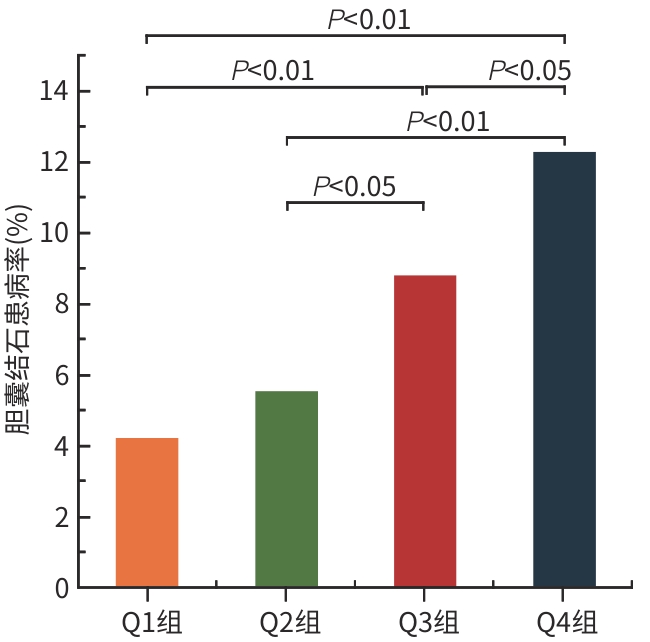
目的 本研究旨在探讨甘油三酯-葡萄糖(TyG)指数与女性胆囊结石患病之间的关联性,并评估其作为女性胆囊结石流行病学筛查指标的可行性。 方法 选择苏北人民医院2021年1月—2023年6月体检的22 979例成年女性,根据腹部彩色多普勒超声仪报告结果将参与者分成胆囊结石组(n=1 763)和非胆囊结石组(n=21 216)。对于符合正态分布的计量资料两组间对比采用成组t检验;非正态分布的计量资料两组间比较采用Mann-Whitney U检验。计数资料两组间比较采用χ²检验。多因素Logistic回归分析、限制性立方样条分析、亚组分析与中介效应被用于探讨TyG与女性胆囊结石患病风险之间的关联性。 结果 女性胆囊结石总体患病率为7.7%。胆囊结石组的年龄、BMI、空腹血糖、TG、TyG指数、TC、Hb、尿素氮、尿酸、血肌酐、TBil、LDL-C水平均高于非胆囊结石组(P值均<0.05),且患有糖尿病、脂肪肝、高血压和高尿酸血症的女性体检人群更易患有胆囊结石(P值均<0.05)。多因素Logistic回归显示,TyG指数四分位组中Q3(8.97~9.38)和Q4(≥9.38)组胆囊结石患病风险分别是Q1(<8.63)组的1.38倍(95%CI:1.15~1.62,P<0.001)和1.39倍(95%CI:1.16~1.68,P<0.001)。调整所有协变量后,TyG指数连续变量也显示与胆囊结石患病风险呈独立正相关(OR=1.24,95%CI:1.11~1.39,P=0.004)。限制性立方样条曲线揭示了TyG指数与胆囊结石发生风险之间存在显著非线性关联(P for nonlinear=0.008),且阈值分析显示,TyG指数在拐点8.95以下部分的效应具有显著统计学意义(OR=1.34,95%CI:1.15~1.97,P=0.042)。亚组分析显示,BMI<25 kg/m2、年龄<50岁、年龄≥50岁、无糖尿病、无脂肪肝、TC<5.72 mmol/L、TBil<21 μmol/L、Hb 110~150 g/L、BUN<7.5 μmol/L、有高血压、无高血压的女性人群中,其TyG指数与胆囊结石之间呈显著正相关(P值均<0.05)。对交互作用P值具有统计学意义的亚组进行了中介分析,结果显示,在TyG指数对胆囊结石的影响中,BMI占中介效应的23.0%,脂肪肝占15.7%,糖尿病占21.0%。 结论 在女性人群中,较高的TyG指数提示更高的胆囊结石风险。降低TyG指数或许可以通过改善胰岛素敏感性,从而减少胆囊结石的风险。 Abstract:Objective To investigate the association between triglyceride-glucose (TyG) index and the prevalence of gallstones in women, and to assess whether it can be used as a convenient indicator for the epidemiological survey of gallstones in women. Methods A total of 22 979 adult women who underwent physical examination in Subei People’s Hospital of Jiangsu from January 2021 to June 2023 were enrolled, and according to the results of abdominal color Doppler ultrasound, they were divided into gallstone group with 1 763 women and non-gallstone group with 21 216 women. The independent samples t-test was used for comparison of normally distributed continuous data between groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between groups; the chi-square test was used for comparison of categorical data between groups. The multivariate logistic regression analysis, the restricted cubic spline analysis, the subgroup analysis, and mediating effect were used to investigate the association between TyG index and the risk of gallstones in women. Results The overall prevalence rate of gallstones was 7.7% in women. Compared with the non-gallstone group, the gallstone group had significantly higher age, BMI, FPG, TG, TyG index, TC, Hb, BUN, UA, SCr, TC, and LDL-C (all P<0.05), and the women with diabetes, fatty liver, hypertension, and hyperuricemia were more likely to have gallstones (all P<0.05). The multivariate logistic regression analysis showed that based on the quartiles of TyG index, the risk of gallstones in the Q3 (8.97 — 9.38) group was 1.38 (95% confidence interval [CI]: 1.15 — 1.62, P<0.001) times that in the Q1 (<8.63) group, and the risk of gallstones in the Q4 (≥9.38) group was 1.39 (95%CI: 1.16 — 1.68, P<0.001) times that in the Q1 group. After adjustment for all covariates, TyG index, as a continuous variable, showed an independent positive correlation with the risk of gallstones (odds ratio [OR]=1.24, 95%CI: 1.11 — 1.39, P=0.004). The restricted cubic spline curve revealed a significant nonlinear association between TyG index and the risk of gallstones (P for non linear=0.008), and the threshold analysis showed statistical significance in the effect of TyG index below the inflection point of 8.95 (OR=1.34, 95%CI: 1.15 — 1.97, P=0.042). The subgroup analysis showed that TyG index was significantly positively correlated with gallstones in women with a BMI of<25 kg/m², an age of<50 years, an age of ≥50 years, the absence of diabetes or fatty liver, total cholesterol<5.72 mmol/L, total bilirubin<21 μmol/L, a hemoglobin level of 110 — 150 g/L, and blood urea nitrogen<7.5 μmol/L (all P<0.05). A mediating analysis was performed for the subgroups with a statistically significant P value for interaction, and the results showed that BMI accounted for 23.0% of the mediating effect in the influence of TyG index on gallstones, and fatty liver and diabetes accounted for 15.7% and 21.0%, respectively. Conclusion In women, a higher TyG index indicates a higher risk of gallstones. Lowering TyG index may reduce the risk of gallstones by improving insulin sensitivity. -
Key words:
- Triglyceride Glucose Index /
- Gallstones /
- Insulin Resistance /
- Cross-Sectional Studies
-
表 1 胆囊结石组和非胆囊结石组的一般资料比较
Table 1. Comparison of general data between gallstone and non-gallstone groups
变量 胆囊结石组(n=1 763) 非胆囊结石组(n=21 216) 统计值 P值 年龄(岁) 50.95±14.51 42.80±13.92 t=23.552 <0.001 BMI(kg/m2) 23.79±3.23 22.61±3.06 t=15.439 <0.001 FPG(mmol/L) 5.09(4.76~5.56) 4.90(4.62~5.25) Z=14.057 <0.001 TG(mmol/L) 1.23(0.87~1.74) 0.98(0.72~1.42) Z=15.869 <0.001 LDL-C(mmol/L) 2.96±0.78 2.79±0.78 t=9.046 <0.001 TyG 9.27±0.60 9.02±0.58 t=17.569 <0.001 TBil(μmol/L) 10.36±4.90 10.07±4.88 t=2.386 0.017 Hb(g/L) 134.19±11.55 132.61±11.69 t=5.472 <0.001 BUN(mmol/L) 4.96±1.29 4.81±1.23 t=5.019 <0.001 UA(μmol/L) 281.52±65.84 266.51±61.06 t=9.855 <0.001 SCr(μmol/L) 67.85±10.55 66.69±9.73 t=4.795 <0.001 TC(mmol/L) 4.79±0.89 4.59±0.90 t=8.736 <0.001 脂肪肝[例(%)] 564(31.99) 3 567(16.81) χ2=254.310 <0.001 糖尿病[例(%)] 121(6.86) 562(2.65) χ2=100.245 <0.001 高尿酸血症[例(%)] 198(11.23) 1 482(6.99) χ2=43.296 <0.001 高血压[例(%)] 373(21.21) 3 182(15.00) χ2=48.079 <0.001 表 2 TyG指数与女性胆囊结石患病的相关性
Table 2. The correlation between the TyG index and the prevalence of gallstones in women
变量 模型1 模型2 模型3 OR(95%CI) P值 OR(95%CI) P值 OR(95%CI) P值 TyG 1.94(1.79~2.09) <0.001 1.28(1.17~1.40) <0.001 1.24(1.11~1.39) 0.004 TyG四分位数 Q1组 1.00 1.00 1.00 Q2组 1.32(1.12~1.57) 0.001 1.09(0.91~1.29) 0.352 1.08(0.91~1.29) 0.446 Q3组 2.19(1.87~2.57) <0.001 1.41(1.19~1.66) <0.001 1.38(1.15~1.62) <0.001 Q4组 3.17(2.73~3.70) <0.001 1.57(1.32~1.86) <0.001 1.39(1.16~1.68) <0.001 趋势检验P值 <0.001 <0.001 <0.001 -
[1] WANG X, YU WQ, JIANG GH, et al. Global epidemiology of gallstones in the 21st century: A systematic review and meta-analysis[J]. Clin Gastroenterol Hepatol, 2024, 22( 8): 1586- 1595. DOI: 10.1016/j.cgh.2024.01.051. [2] LAMMERT F, GURUSAMY K, KO CW, et al. Gallstones[J]. Nat Rev Dis Primers, 2016, 2: 16024. DOI: 10.1038/nrdp.2016.24. [3] SIMONSEN MH, ERICHSEN R, FRØSLEV T, et al. Postmenopausal estrogen therapy and risk of gallstone disease: A population-based case-control study[J]. Drug Saf, 2013, 36( 12): 1189- 1197. DOI: 10.1007/s40264-013-0118-7. [4] SUN XH, WANG YJ, ZHANG W, et al. Epidemiological characteristics, diagnosis, treatment and prognosis of gallbladder cancer in China: A report of 6 159 cases[J]. Chin J Dig Surg, 2022, 21( 1): 114- 128. DOI: 10.3760/cma.j.cn115610-20220103-00004.孙旭恒, 王一钧, 张薇, 等. 中国胆囊癌流行病学特征与诊治及预后分析(附6 159例报告)[J]. 中华消化外科杂志, 2022, 21( 1): 114- 128. DOI: 10.3760/cma.j.cn115610-20220103-00004. [5] ZHU Q, XING YW, FU YF, et al. Causal association between metabolic syndrome and cholelithiasis: A Mendelian randomization study[J]. Front Endocrinol(Lausanne), 2023, 14: 1180903. DOI: 10.3389/fendo.2023.1180903. [6] SUN YT, JI HY, SUN WJ, et al. Triglyceride glucose(TyG) index: A promising biomarker for diagnosis and treatment of different diseases[J]. Eur J Intern Med, 2025, 131: 3- 14. DOI: 10.1016/j.ejim.2024.08.026. [7] LUO PP, LIU Q, HUANG LW. Predictive value of triglyceride-glucose body mass index(TyG-BMI) for the severity of hyperlipidemic acute pancreatitis[J]. J Clin Hepatol, 2024, 40( 8): 1661- 1665. DOI: 10.12449/JCH240824.罗萍萍, 刘群, 黄丽雯. 甘油三酯葡萄糖体质量指数(TyG-BMI)对高脂血症性急性胰腺炎严重程度的预测价值[J]. 临床肝胆病杂志, 2024, 40( 8): 1661- 1665. DOI: 10.12449/JCH240824. [8] LYU JT, LIN QH, FANG ZB, et al. Complex impacts of gallstone disease on metabolic syndrome and nonalcoholic fatty liver disease[J]. Front Endocrinol(Lausanne), 2022, 13: 1032557. DOI: 10.3389/fendo.2022.1032557. [9] CAMPOREZ JP, LYU K, GOLDBERG EL, et al. Anti-inflammatory effects of oestrogen mediate the sexual dimorphic response to lipid-induced insulin resistance[J]. J Physiol, 2019, 597( 15): 3885- 3903. DOI: 10.1113/JP277270. [10] STUBBINS RE, NAJJAR K, HOLCOMB VB, et al. Oestrogen alters adipocyte biology and protects female mice from adipocyte inflammation and insulin resistance[J]. Diabetes Obes Metab, 2012, 14( 1): 58- 66. DOI: 10.1111/j.1463-1326.2011.01488.x. [11] TAHAPARY DL, PRATISTHITA LB, FITRI NA, et al. Challenges in the diagnosis of insulin resistance: Focusing on the role of HOMA-IR and Tryglyceride/glucose index[J]. Diabetes Metab Syndr, 2022, 16( 8): 102581. DOI: 10.1016/j.dsx.2022.102581. [12] The Editorial Board of“Clinical Guide for the Prevention and Treatment of Geriatric Diabetes in China”. Clinical guide for the prevention and treatment of type 2 diabetes in elderly Chinese(2022 Edition)[J]. Chin J Diabetes, 2022, 30( 1): 2- 51. DOI: 10.3969/j.issn.1006-6187.2022.01.002.《中国老年型糖尿病防治临床指南》编写组. 中国老年2型糖尿病防治临床指南(2022年版)[J]. 中国糖尿病杂志, 2022, 30( 1): 2- 51. DOI: 10.3969/j.issn.1006-6187.2022.01.002. [13] Chinese Medical Doctor Association, Branch Nephrology. Practice guidelines for the diagnosis and treatment of hyperuricemia in kidney disease in China(2017 Edition)[J]. Nat Med J China, 2017, 97( 25): 1927- 1936. DOI: 10.3760/cma.j.issn.0376-2491.2017.25.003.中国医师协会肾脏内科医师分会. 中国肾脏疾病高尿酸血症诊治的实践指南(2017版)[J]. 中华医学杂志, 2017, 97( 25): 1927- 1936. DOI: 10.3760/cma.j.issn.0376-2491.2017.25.003. [14] Editorial Board of Chinese Journal of Digestion, Hepatobiliary Disease Cooperation Group of Chinese Society of Gastroenterology. Consensus on diagnosis and treatment of chronic cholecystitis and gallstones in China(2018)[J]. J Clin Hepatol, 2019, 35( 6): 1231- 1236. DOI: 10.3969/j.issn.1001-5256.2019.06.11.中华消化杂志编辑委员会, 中华医学会消化病学分会肝胆疾病协作组. 中国慢性胆囊炎、胆囊结石内科诊疗共识意见(2018年)[J]. 临床肝胆病杂志, 2019, 35( 6): 1231- 1236. DOI: 10.3969/j.issn.1001-5256.2019.06.11. [15] Chinese Society of Hepatology. Guidelines for the prevention and treatment of metabolic dysfunction-associated(Non-Alcoholic) fatty liver disease(2024 Edition)[J]. J Prac Hepatol, 2024, 27( 4): 494- 510. DOI: 10.3760/cma.j.cn501113-20240327-00163.中华医学会肝病学分会. 代谢相关(非酒精性)脂肪性肝病防治指南(2024年版)[J]. 实用肝脏病杂志, 2024, 27( 4): 494- 510. DOI: 10.3760/cma.j.cn501113-20240327-00163. [16] LI CY, ZHU P, JIAO P, et al. Association between triglyceride-glucose index and the risk of gallstone disease: A multicenter health check-up population study[J]. Modern Prevent Med, 2023, 50( 5): 775- 780, 802. DOI: 10.20043/j.cnki.MPM.202211404.李春燕, 朱培, 焦鹏, 等. 甘油三酯-葡萄糖指数与胆石病患病风险关联——多中心健康体检人群研究[J]. 现代预防医学, 2023, 50( 5): 775- 780, 802. DOI: 10.20043/j.cnki.MPM.202211404. [17] GONG L, FAN SJ, PENG ZF, et al. The association between triglyceride-glucose index and gallstones: NHANES 2017-2020[J]. Front Endocrinol(Lausanne), 2024, 15: 1437711. DOI: 10.3389/fendo.2024.1437711. [18] LI HL, ZHANG CF. Association between triglyceride-glucose index and gallstones: A cross-sectional study[J]. Sci Rep, 2024, 14( 1): 17778. DOI: 10.1038/s41598-024-68841-6. [19] FENG XY, WU SW, KE B, et al. Elevated TyG index associated with increased prevalence of gallstones in a United States cross-sectional study[J]. Front Public Health, 2024, 12: 1351884. DOI: 10.3389/fpubh.2024.1351884. [20] Branch of Biliary Surgery Chinese Surgical Society, Chinese Committee of Biliary Surgeons. Guideline for the diagnosis and treatment of gallbladder carcinoma(2019 edition)[J]. Chin J Surg, 2020, 58( 4): 243- 251. DOI: 10.3760/cma.j.cn112139-20200106-00014.中华医学会外科学分会胆道外科学组, 中国医师协会外科医师分会胆道外科专业委员会. 胆囊癌诊断和治疗指南(2019版)[J]. 中华外科杂志, 2020, 58( 4): 243- 251. DOI: 10.3760/cma.j.cn112139-20200106-00014. [21] BIDDINGER SB, HAAS JT, YU BB, et al. Hepatic insulin resistance directly promotes formation of cholesterol gallstones[J]. Nat Med, 2008, 14( 7): 778- 782. DOI: 10.1038/nm1785. [22] ZHU Q, SUN XB, JI XK, et al. The association between gallstones and metabolic syndrome in urban Han Chinese: A longitudinal cohort study[J]. Sci Rep, 2016, 6: 29937. DOI: 10.1038/srep29937. [23] CAZZO E, GESTIC MA, UTRINI MP, et al. Influence of insulin resistance status on the development of gallstones following roux-en-Y gastric bypass: A prospective cohort study[J]. Obes Surg, 2016, 26( 4): 769- 775. DOI: 10.1007/s11695-015-1815-3. [24] NERVI F, MIQUEL JF, ALVAREZ M, et al. Gallbladder disease is associated with insulin resistance in a high risk Hispanic population[J]. J Hepatol, 2006, 45( 2): 299- 305. DOI: 10.1016/j.jhep.2006.01.026. [25] HYOGO H, ROY S, PAIGEN B, et al. Leptin promotes biliary cholesterol elimination during weight loss in ob/ob mice by regulating the enterohepatic circulation of bile salts[J]. J Biol Chem, 2002, 277( 37): 34117- 34124. DOI: 10.1074/jbc.M203912200. [26] WEN J, JIANG Y, LEI ZM, et al. Leptin influence cholelithiasis formation by regulating bile acid metabolism[J]. Turk J Gastroenterol, 2021, 32( 1): 97- 105. DOI: 10.5152/tjg.2020.19594. [27] TAKEUCHI T, KUBOTA T, NAKANISHI Y, et al. Gut microbial carbohydrate metabolism contributes to insulin resistance[J]. Nature, 2023, 621( 7978): 389- 395. DOI: 10.1038/s41586-023-06466-x. [28] WANG QH, JIAO L, HE CQ, et al. Alteration of gut microbiota in association with cholesterol gallstone formation in mice[J]. BMC Gastroenterol, 2017, 17( 1): 74. DOI: 10.1186/s12876-017-0629-2. [29] LAVOIE JM. Dynamics of hepatic and intestinal cholesterol and bile acid pathways: The impact of the animal model of estrogen deficiency and exercise training[J]. World J Hepatol, 2016, 8( 23): 961- 975. DOI: 10.4254/wjh.v8.i23.961. [30] DE PAOLI M, ZAKHARIA A, WERSTUCK GH. The role of estrogen in insulin resistance: A review of clinical and preclinical data[J]. Am J Pathol, 2021, 191( 9): 1490- 1498. DOI: 10.1016/j.ajpath.2021.05.011. [31] YANG SJ, YU B, YU WQ, et al. Development and validation of an age-sex-ethnicity-specific metabolic syndrome score in the Chinese adults[J]. Nat Commun, 2023, 14( 1): 6988. DOI: 10.1038/s41467-023-42423-y. [32] FAHED G, AOUN L, ZERDAN M BOU, et al. Metabolic syndrome: Updates on pathophysiology and management in 2021[J]. Int J Mol Sci, 2022, 23( 2): 786. DOI: 10.3390/ijms23020786. -



 PDF下载 ( 1413 KB)
PDF下载 ( 1413 KB)

 下载:
下载: