失代偿期乙型肝炎肝硬化患者再代偿的影响因素分析
DOI: 10.12449/JCH250721
Influencing factors for recompensation in patients with decompensated hepatitis B cirrhosis
-
摘要:
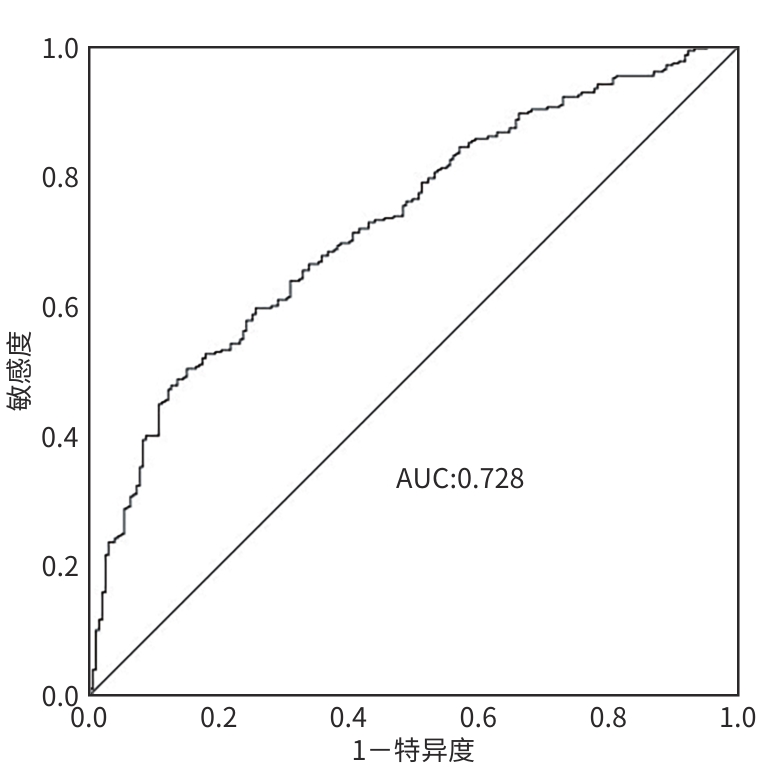
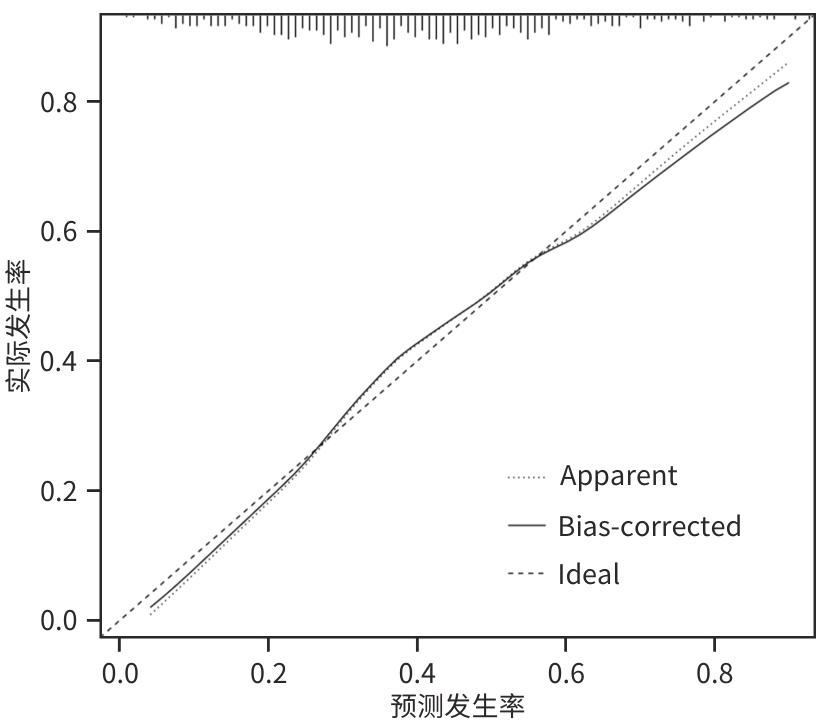
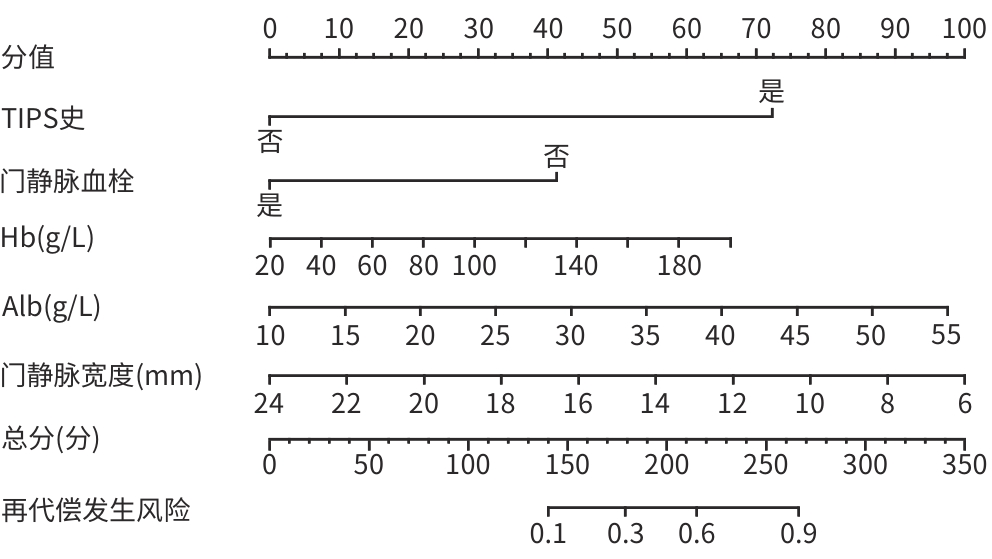
目的 研究失代偿期乙型肝炎硬化患者再代偿发生的影响因素,建立预测模型。 方法 收集2016年1月1日—2022年12月31日就诊于昆明市第三人民医院并诊断为失代偿期乙型肝炎肝硬化的患者517例。查阅患者资料,至少1年内无门静脉高压相关并发症者纳入再代偿组(n=207),未再代偿者为持续失代偿组(n=310)。收集相关临床资料,对可能影响再代偿发生的因素进行单因素及多因素Cox回归模型分析。符合正态分布的计量资料,两组间比较采用成组t检验。不符合正态分布的计量资料,两组间比较采用Mann-Whitney U检验。计数资料两组间比较采用χ²检验或Fisher确切概率法。使用“rms”程序包建立列线图;绘制受试者操作特征曲线(ROC曲线)并计算曲线下面积;使用Hosmer-Lemeshow检验评估模型的拟合度;使用“Calibration Curves”程序包绘制校准曲线对模型进行评价。 结果 失代偿期乙型肝炎肝硬化患者中有207例(40.03%)发生再代偿。单因素Cox回归分析结果显示,再代偿组经颈静脉肝内门体分流术(TIPS)史、基因分型、门静脉血栓、合并感染、Child-Pugh分级、年龄、Hb、PLT、总蛋白、Alb、ALT、TG、甘油三酯、肌酐、Na、IL-6、超敏C反应蛋白、门静脉宽度、门静脉流速与持续失代偿组差异均有统计学意义(P值均<0.05)。多因素回归分析结果显示:TIPS史(HR=2.491,95%CI:1.325~4.681,P=0.005)、门静脉血栓形成(HR=0.345,95%CI:0.152~0.783,P=0.001)、Hb(HR=1.007,95%CI:1.000~1.013,P=0.028)、Alb(HR=1.048,95%CI:1.017~1.080,P=0.002)和门静脉宽度(HR=0.899,95%CI:0.835~0.967,P=0.004)是失代偿期乙型肝炎肝硬化患者再代偿的独立影响因素;基于以上5个影响因素构建列线图,Hosmer-Lemesho检验显示,该模型具有较好的拟合度(χ²=3.202,P=0.921),该模型的ROC曲线下面积为0.728,敏感度为50.3%,特异度为85.0%,校准曲线显示该模型预测失代偿期乙型肝炎肝硬化患者再代偿发生的预测值与实际值有较好的一致性。 结论 有TIPS史、Alb及Hb水平高的失代偿期乙型肝炎肝硬化患者更容易出现再代偿,合并门静脉血栓及门静脉宽度增加的患者不易出现再代偿。 Abstract:Objective To investigate the influencing factors for recompensation in patients with decompensated hepatitis B cirrhosis, and to establish a predictive model. Methods A total of 517 patients who attended The Third People’s Hospital of Kunming and were diagnosed with decompensated hepatitis B cirrhosis from January 1, 2016 to December 31, 2022 were enrolled. The clinical data of the patients were reviewed, and the 207 patients with no portal hypertension-related complications within at least 1 year were enrolled as recompensation group, while the 310 patients without recompensation were enrolled as persistent decompensation group. Related clinical data were collected, and the univariate and multivariate Cox regression analyses were performed for the factors that might affect the occurrence of recompensation. The independent-samples t test was used for comparison of normally distributed continuous data between two groups, and the Mann-Whitney U test was used for comparison of non-normally distributed continuous data between two groups; the chi-square test or the Fisher’s exact test was used for comparison of categorical data between two groups. The “rms” package was used to establish a nomogram; the receiver operating characteristic (ROC) curve was plotted, and the area under the ROC curve (AUC) was calculated; the Hosmer-Lemeshow test was used to evaluate the degree of fitting of the model; the “Calibration Curves” package was used to plot the calibration curve for model assessment. Results Among the patients with decompensated hepatitis B cirrhosis, 207 (40.03%) had recompensation. The univariate Cox regression analysis showed that there were significant differences between the recompensation group and the persistent decompensation group in TIPS history, genotyping, portal vein thrombosis, complicated infection, Child-Pugh class, age, hemoglobin (Hb), platelet count, total protein, albumin (Alb), alanine aminotransferase, triglyceride, cholesterol, creatinine, Na, interleukin-6, high-sensitivity C-reactive protein, portal vein width, and portal vein velocity (all P<0.05). The multivariate regression analysis showed that TIPS history (hazard ratio [HR]=2.491, 95% confidence interval [CI]: 1.325 — 4.681, P=0.005), portal vein thrombosis (HR=0.345, 95%CI: 0.152 — 0.783, P=0.001), Hb (HR=1.007, 95%CI: 1.000 — 1.013, P=0.028), Alb (HR=1.048, 95%CI: 1.017 — 1.080, P=0.002), and portal vein width (HR=0.899, 95%CI: 0.835 — 0.967, P=0.004) were independent influencing factors for recompensation in patients with decompensated hepatitis B cirrhosis. A nomogram model was established based on the above five influencing factors, and the Hosmers-Lemeshow test showed that this model had a good degree of fitting (χ²=3.202, P=0.921). The nomogram model had an AUC of 0.728, a sensitivity of 50.3%, and a specificity of 85.0%, and the calibration curve showed good consistency between the actual value of this model in predicting the occurrence of recompensation and the predicted value in patients with decompensated hepatitis B cirrhosis. Conclusion Patients with decompensated hepatitis B cirrhosis who have a history of TIPS and high levels of Alb and Hb are more likely to have recompensation, and it is relatively difficult for patients with portal vein thrombosis and an increase in portal vein width to achieve recompensation. -
Key words:
- Hepatitis B, Chronic /
- Liver Cirrhosis /
- Risk Factors
-
表 1 再代偿组与持续失代偿组一般资料比较
Table 1. Comparison of general information between the redecompensation group and the continuing decompensation group
项目 再代偿组(n=207) 持续失代偿组(n=310) 统计值 P值 男[例(%)] 146(70.5) 236(76.1) χ²=2.016 0.156 年龄(岁) 50.38±9.85 52.66±11.14 t=-2.387 0.066 BMI(kg/m²) 22.75(21.56~24.02) 22.86(21.87~24.27) Z=-1.073 0.283 2型糖尿病史[例(%)] 30(14.5) 42(13.5) χ²=0.092 0.761 高血压病史[例(%)] 29(14.0) 25(8.1) χ²=4.690 0.030 TIPS史[例(%)] 11(5.3) 2(0.6) χ²=11.037 0.001 部分脾栓塞史[例(%)] 20(9.7) 19(6.1) χ²=2.221 0.136 内镜治疗史[例(%)] 33(15.9) 57(18.4) χ²=0.516 0.473 口服NSBB[例(%)] 27(13.0) 23(7.4) χ²=4.494 0.034 门静脉血栓[例(%)] 6(2.9) 36(11.6) χ²=12.628 <0.001 肝癌家族史[例(%)] 15(7.2) 19(6.1) χ²=0.252 0.616 SVR[例(%)] 195(94.2) 282(91.0) χ²=1.820 0.177 感染[例(%)] 62(30.0) 136(43.9) χ²=10.177 0.001 腹水分级[例(%)] χ²=2.936 0.230 无 15(7.2) 14(4.5) 少量 116(56.0) 164(52.9) 中大量 76(36.7) 132(42.6) Child-Pugh分级[例(%)] χ²=18.148 <0.001 A级 51(24.6) 34(11.0) B级 92(44.4) 147(47.4) C级 64(30.9) 129(41.6) 基因分型[例(%)] χ²=9.411 0.009 C型 76(36.7) 93(30.0) B型 29(14.0) 25(8.1) 未测 102(49.3) 192(61.9) WBC(×109/L) 3.86(3.02~5.44) 3.94(2.83~5.25) Z=-0.400 0.689 Hb(g/L) 127.18±25.14 114.25±29.88 t=5.131 0.021 PLT(×109/L) 86.00(60.00~115.00) 73.50(52.75~104.25) Z=-2.695 0.007 TBil(mmol/L) 31.80(21.30~60.10) 34.00(21.08~66.03) Z=-0.158 0.875 AST(U/L) 55.00(35.00~98.00) 54.00(37.75~100.25) Z=-0.147 0.883 ALT(U/L) 38.00(25.00~83.00) 39.00(26.00~66.25) Z=-0.768 0.443 TP(g/L) 63.12±8.60 60.96±8.32 t=2.843 0.929 Alb(g/L) 32.30(28.00~37.20) 28.65(25.30~33.22) Z=-0.857 <0.001 TG(mmol/L) 0.81(0.60~1.13) 0.72(0.51~1.01) Z=-2.367 0.018 CHOL(mmol/L) 3.42(2.91~3.94) 3.17(2.46~3.85) Z=-2.903 0.004 Cr(μmol/L) 63.00(52.00~74.60) 64.90(54.00~78.00) Z=-1.562 0.118 Na(mmol/L) 139.90(137.80~141.70) 138.9(136.88~140.80) Z=-3.304 0.001 hs-CRP(mg/L) 4.09(1.63~10.58) 6.01(1.96~15.14) Z=-2.562 0.010 IL-6(pg/mL) 11.49(7.93~20.10) 16.69(8.60~30.79) Z=-3.634 <0.001 PT(s) 16.80(15.80~18.80) 17.50(15.70~19.70) Z=-2.195 0.028 APTT(s) 43.14±6.96 42.92±7.05 t=0.336 0.737 AFP(ng/mL) 8.40(3.32~54.19) 7.28(2.97~26.57) Z=-1.741 0.082 超声弹性成像(kPa) 18.04(15.42~26.35) 18.17(14.79~21.60) Z=-0.637 0.524 门静脉宽度(mm) 11.00(10.00~12.00) 12.00(10.80~13.20) Z=-3.989 <0.001 门静脉流速(cm/s) 14.80(12.70~18.30) 14.18(11.98~16.42) Z=-2.651 0.008 表 2 Cox回归分析失代偿期乙型肝炎肝硬化患者再代偿的影响因素
Table 2. Cox regression analysis of factors affecting recompensation in patients with decompensated hepatitis B cirrhosis
项目 单因素分析 多因素分析 HR 95%CI P值 HR 95%CI P值 性别 1.204 0.893~1.623 0.224 2型糖尿病史 0.960 0.652~1.414 0.836 高血压病史 0.687 0.464~1.017 0.061 TIPS史 0.416 0.226~0.764 0.005 2.491 1.325~4.681 0.005 部分脾栓塞史 0.746 0.470~1.183 0.212 内镜治疗史 1.157 0.798~1.679 0.442 口服NBBS 0.701 0.468~1.050 0.085 基因分型 C型 1.000 未测 0.721 0.536~0.970 0.031 B型 1.263 0.823~1.937 0.285 门静脉血栓 3.443 1.528~7.758 0.003 0.345 0.152~0.783 0.001 腹水分级 中大量 1.000 无 1.494 0.859~2.600 0.155 少量 1.159 0.868~1.548 0.317 合并感染 1.518 1.128~2.044 0.006 肝癌家族史 0.877 0.518~1.483 0.624 SVR 0.695 0.388~1.245 0.221 Child-Pugh分级 C级 1.000 A级 1.584 1.096~2.288 0.014 B级 1.181 0.858~1.625 0.306 年龄 0.986 0.973~0.998 0.027 BMI 0.970 0.913~1.030 0.317 WBC 0.981 0.935~1.028 0.418 Hb 1.012 1.007~1.017 <0.001 1.007 1.000~1.013 0.028 PLT 1.004 1.001~1.006 0.005 TBil 1.000 0.998~1.001 0.676 AST 1.000 1.000~1.001 0.206 ALT 1.001 1.000~1.001 0.006 TP 1.023 1.006~1.040 0.007 Alb 1.053 1.033~1.073 <0.001 1.048 1.017~1.080 0.002 TG 1.326 1.065~1.651 0.012 CHOL 1.153 1.040~1.278 0.007 Cr 0.993 0.987~0.999 0.029 Na 1.062 1.017~1.108 0.006 hs-CRP 0.985 0.974~0.996 0.008 IL-6 0.993 0.988~0.998 0.010 PT 0.956 0.910~1.004 0.071 APTT 1.005 0.985~1.024 0.648 AFP 1.000 0.999~1.001 0.982 超声弹性成像 0.999 0.979~1.020 0.947 门静脉宽度 0.887 0.827~0.951 0.001 0.899 0.835~0.967 0.004 门静脉流速 1.048 1.004~1.094 0.033 -
[1] MENG Y, XU BQ, FU ZG, et al. Cytoplasmic EpCAM over-expression is associated with favorable clinical outcomes in pancreatic cancer patients with Hepatitis B virus negative infection[J]. Int J Clin Exp Med, 2015, 8( 12): 22204- 22216. [2] YIP VSK, POON RTP, CHOK KSH, et al. Comparison of survival outcomes between right posterior sectionectomy and right hepatectomy for hepatocellular carcinoma in cirrhotic liver: A single-centre experience[J]. World J Surg, 2015, 39( 11): 2764- 2770. DOI: 10.1007/s00268-015-3146-x. [3] LIAW YF, SHEEN IS, LEE CM, et al. Tenofovir disoproxil fumarate(TDF), emtricitabine/TDF, and entecavir in patients with decompensated chronic hepatitis B liver disease[J]. Hepatology, 2011, 53( 1): 62- 72. DOI: 10.1002/hep.23952. [4] LIAW YF, RAPTOPOULOU-GIGI M, CHEINQUER H, et al. Efficacy and safety of entecavir versus adefovir in chronic hepatitis B patients with hepatic decompensation: A randomized, open-label study[J]. Hepatology, 2011, 54( 1): 91- 100. DOI: 10.1002/hep.24361. [5] SRIVASTAVA M, RUNGTA S, DIXIT VK, et al. Predictors of survival in hepatitis B virus related decompensated cirrhosis on tenofovir therapy: An Indian perspective[J]. Antiviral Res, 2013, 100( 2): 300- 305. DOI: 10.1016/j.antiviral.2013.08.020. [6] RUAN JJ, WEN SF, WANG X, et al. Influencing factors for recompensation in patients with first-time decompensated hepatitis B cirrhosis[J]. J Clin Hepatol, 2022, 38( 8): 1796- 1800. DOI: 10.3969/j.issn.1001-5256.2022.08.015.阮佳佳, 温世飞, 王霞, 等. 首次失代偿期乙型肝炎肝硬化患者获得再代偿的影响因素分析[J]. 临床肝胆病杂志, 2022, 38( 8): 1796- 1800. DOI: 10.3969/j.issn.1001-5256.2022.08.015. [7] Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the management of ascites in cirrhosis(2023 version)[J]. Chin J Hepatol, 2023, 31( 8): 813- 826. DOI: 10.3760/cma.j.cn501113-20230719-00011.中华医学会肝病学分会. 肝硬化腹水诊疗指南(2023年版)[J]. 中华肝脏病杂志, 2023, 31( 8): 813- 826. DOI: 10.3760/cma.j.cn501113-20230719-00011. [8] KIM TH, UM SH, LEE YS, et al. Determinants of re-compensation in patients with hepatitis B virus-related decompensated cirrhosis starting antiviral therapy[J]. Aliment Pharmacol Ther, 2022, 55( 1): 83- 96. DOI: 10.1111/apt.16658. [9] WANG Q, ZHAO H, DENG Y, et al. Validation of Baveno VII criteria for recompensation in entecavir-treated patients with hepatitis B-related decompensated cirrhosis[J]. J Hepatol, 2022, 77( 6): 1564- 1572. DOI: 10.1016/j.jhep.2022.07.037. [10] ZHANG T, DENG Y, KANG HY, et al. Recompensation of complications in patients with hepatitis B virus-related decompensated cirrhosis treated with entecavir antiviral therapy[J]. Chin J Hepatol, 2023, 31( 7): 692- 697. DOI: 10.3760/cma.j.cn501113-20230324-00126.张婷, 邓优, 康海燕, 等. 恩替卡韦抗病毒治疗的乙型肝炎失代偿期肝硬化患者并发症的再代偿[J]. 中华肝脏病杂志, 2023, 31( 7): 692- 697. DOI: 10.3760/cma.j.cn501113-20230324-00126. [11] D’AMICO G, GARCIA-TSAO G, PAGLIARO L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies[J]. J Hepatol, 2006, 44( 1): 217- 231. DOI: 10.1016/j.jhep.2005.10.013. [12] REIBERGER T, HOFER BS. The Baveno VII concept of cirrhosis recompensation[J]. Dig Liver Dis, 2023, 55( 4): 431- 441. DOI: 10.1016/j.dld.2022.12.014. [13] COOL J, ROSENBLATT R, KUMAR S, et al. Portal vein thrombosis prevalence and associated mortality in cirrhosis in a nationally representative inpatient cohort[J]. J Gastroenterol Hepatol, 2019, 34( 6): 1088- 1092. DOI: 10.1111/jgh.14501. [14] ZHANG Y, XU BY, WANG XB, et al. Prevalence and clinical significance of portal vein thrombosis in patients with cirrhosis and acute decompensation[J]. Clin Gastroenterol Hepatol, 2020, 18( 11): 2564- 2572. e 1. DOI: 10.1016/j.cgh.2020.02.037. [15] XIAN JC, TANG YZ, SHAO H, et al. Effect of portal vein thrombosis on the prognosis of patients with cirrhosis without a liver transplant: A systematic review and meta-analysis[J]. Medicine(Baltimore), 2021, 100( 16): e25439. DOI: 10.1097/MD.0000000000025439. [16] LI MB. Analysis of cirrhosis recompensation after TIPS and its predictive factors[D]. Taiyuan: Shanxi Medical University, 2023.李满彪. TIPS术后肝硬化再代偿及其预测因素分析[D]. 太原: 山西医科大学, 2023. [17] MANEKELLER S, KALFF JC. Esophageal variceal bleeding: Management and tips on transjugular intrahepatic portosystemic shunt[J]. Chirurg, 2019, 90( 8): 614- 620. DOI: 10.1007/s00104-019-0949-6. [18] LV Y, BAI W, LI K, et al. Anticoagulation and transjugular intrahepatic portosystemic shunt for the management of portal vein thrombosis in cirrhosis: A prospective observational study[J]. Am J Gastroenterol, 2021, 116( 7): 1447- 1464. DOI: 10.14309/ajg.0000000000001194. [19] SÁNCHEZ J, GONZÁLEZ S, POYATOS P, et al. Recompensation after TIPS reduces the incidence of hepatocellular carcinoma and increases survival in patients with cirrhosis[J]. Liver Int, 2024, 44( 11): 3072- 3082. DOI: 10.1111/liv.16095. [20] ARAVINTHAN AD, BARBAS AS, DOYLE AC, et al. Characteristics of liver transplant candidates delisted following recompensation and predictors of such delisting in alcohol-related liver disease: A case-control study[J]. Transpl Int, 2017, 30( 11): 1140- 1149. DOI: 10.1111/tri.13008. [21] HOFER BS, SIMBRUNNER B, HARTL L, et al. Hepatic recompensation according to Baveno VII criteria is linked to a significant survival benefit in decompensated alcohol-related cirrhosis[J]. Liver Int, 2023, 43( 10): 2220- 2231. DOI: 10.1111/liv.15676. [22] SCHEINER B, SEMMLER G, MAURER F, et al. Prevalence of and risk factors for anaemia in patients with advanced chronic liver disease[J]. Liver Int, 2020, 40( 1): 194- 204. DOI: 10.1111/liv.14229. [23] COLLAS O, ROBERTSON FP, FULLER BJ, et al. Anaemia in patients with chronic liver disease and its association with morbidity and mortality following liver transplantation[J]. Int J Surg, 2018, 53: 48- 52. DOI: 10.1016/j.ijsu.2018.02.053. [24] CAI M, YANG N, LIN S, et al. Anemia predicts poor outcomes in patients with HBV-related decompensated cirrhosis[J]. Clin Lab, 2021, 67( 3). DOI: 10.7754/Clin.Lab.2020.200701. -



 PDF下载 ( 1324 KB)
PDF下载 ( 1324 KB)

 下载:
下载: