原发性胆汁性胆管炎合并干燥综合征的危险因素分析及预测模型构建
DOI: 10.12449/JCH250718
Risk factors and prediction models for primary biliary cholangitis comorbid with Sjögren’s syndrome
-
摘要:
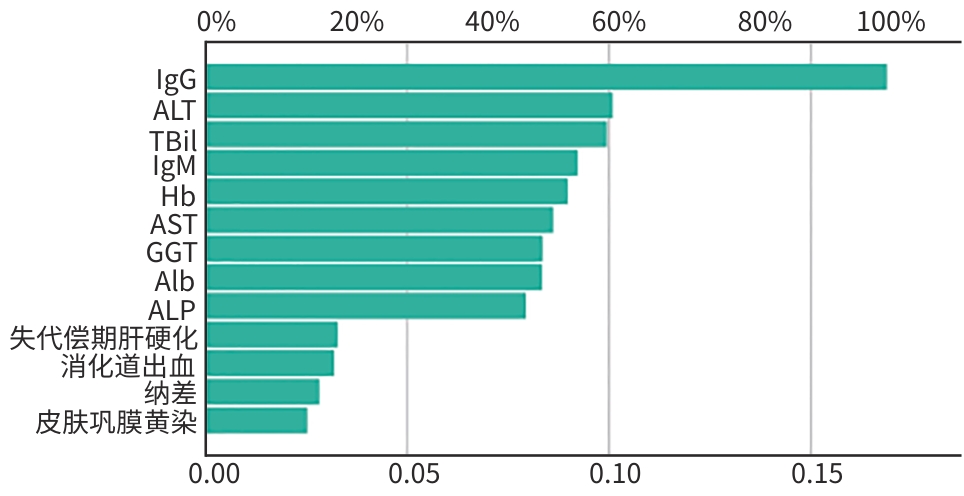
目的 探讨原发性胆汁性胆管炎(PBC)患者合并干燥综合征(SS)的危险因素,建立诊断预测模型并比较不同模型间的效能。 方法 纳入2012年1月—2023年4月在苏州大学附属第一医院首次诊断为PBC的患者183例,并根据是否患有SS将其分为单纯PBC组(n=96)和PBC合并SS组(n=87),比较两组患者的临床表现、血清学抗体、实验室指标。计量资料两组间比较采用成组t检验或Mann-Whitney U检验;计数资料两组间比较采用χ2检验。多因素Logistic回归分析PBC患者合并SS的危险因素。继而建立人工神经网络(ANN)诊断预测模型及多因素逻辑回归(MLR)诊断预测模型,通过MedCalc软件绘制受试者操作特征曲线,采用Delong检验比较两模型曲线下面积(AUC)的差异。 结果 血清免疫球蛋白G水平(OR=1.600,95%CI:1.364~1.876,P<0.001)是PBC患者合并SS的独立危险因素,血清TBil水平(OR=0.760,95%CI:0.700~0.811,P=0.005)是PBC患者合并SS的独立保护因素。PBC合并SS诊断的ANN模型与MLR模型的AUC分别为0.919(95%CI:0.870~0.954)和0.896(95%CI:0.843~0.936),证明两模型预测效能较好,其中ANN模型的预测效能优于MLR模型,两模型效能之间差异具有统计学意义(P=0.019 2)。 结论 PBC合并SS患者首次就诊时常处于病程早期,病情较轻,早期诊治有利于患者的预后。对于首次诊断或就诊期间发现血清免疫球蛋白G偏高的PBC患者,筛查排除SS诊断是有必要的。 Abstract:Objective To investigate the risk factors associated with the coexistence of Sjögren’s syndrome (SS) in patients with primary biliary cholangitis (PBC), and to develop and compare diagnostic prediction models for the comorbidity of the two conditions. Methods A total of 183 patients first diagnosed with PBC at The First Affiliated Hospital of Soochow University from January 2012 to April 2023 were included. They were divided into two groups based on the presence or absence of SS: those with PBC alone(n=96)and those with PBC accompanied by SS(n=87). Clinical manifestations, serological antibody results, and laboratory parameters were compared between the two groups. Continuous data were compared using the t-test or Mann-Whitney U test, while categorical data were compared using the chi-square test. The risk factors for the presence of SS in PBC were identified through a multivariable Logistic regression analysis. Subsequently, an artificial neural network (ANN) model and a multiple logistic regression (MLR) model were constructed to predict the presence of SS in PBS. The receiver operating characteristic curve was plotted in MedCalc, and the area under the curve (AUC) was compared using the Delong test. Results Serum IgG level (odds ratio [OR]=1.600, 95% confidence interval [CI]:1.364 — 1.876,P<0.001) was an independent risk factor, while serum total bilirubin level (OR=0.760,95%CI:0.700 — 0.811,P=0.005) was an independent protective factor against the presence of SS in patients with PBC. The AUCs of the ANN model and the MLR model diagnosing SS in PBC were 0.919 (95%CI:0.870 — 0.954) and 0.896 (95%CI:0.843 — 0.936), respectively, both showing good predictive efficacy, and the predictive efficacy of the ANN model was significantly better than that of the MLR model (P=0.019 2). Conclusion Patients with PBC complicated by SS usually present at an early stage with mild symptoms during their initial medical consultation, when early diagnosis and treatment are beneficial for their prognosis. For patients with PBC showing high serum IgG levels at the first diagnosis or consultation, SS screening is necessary. -
Key words:
- Primary Biliary Cholangitis /
- Sjogren’s Syndrome /
- Risk Factors
-
表 1 PBC合并SS组与单纯PBC组的一般情况及临床特征比较
Table 1. Comparison of general and clinical characteristics between Group PBC combined with SS and Group PBC-only
指标 PBC合并SS组(n=87) 单纯PBC组(n=96) 统计值 P值 女[例(%)] 83(95.4) 89(92.7) χ2=0.586 0.444 年龄(岁) 54.77±11.36 57.28±12.04 t=2.095 0.149 病程(月) 7.00(3.00~16.00) 37.00(14.00~74.00) Z=6.155 <0.001 吸烟史[例(%)] 5(5.75) 6(6.25) χ2=0.020 0.886 饮酒史[例(%)] 3(3.45) 4(4.17) χ2=0.064 0.800 高血压[例(%)] 9(10.34) 10(10.42) χ2=0.000 0.987 糖尿病[例(%)] 10(11.49) 11(11.46) χ2=0.000 0.994 肾脏受累[例(%)] 7(8.05) 9(9.38) χ2=0.101 0.751 乏力[例(%)] 71(81.61) 87(90.63) χ2=3.145 0.076 腹胀不适[例(%)] 45(51.72) 30(31.25) χ2=2.898 0.089 水肿[例(%)] 17(19.54) 22(22.92) χ2=0.310 0.578 肝掌[例(%)] 6(6.90) 3(3.13) χ2=1.388 0.239 蜘蛛痣[例(%)] 7(8.05) 2(2.08) χ2=3.470 0.062 恶心呕吐[例(%)] 10(11.49) 11(11.46) χ2=0.000 0.994 瘙痒[例(%)] 16(18.39) 20(20.83) χ2=0.172 0.618 皮肤巩膜黄染[例(%)] 19(21.84) 48(50.00) χ2=15.596 <0.001 纳差[例(%)] 43(49.43) 73(76.04) χ2=13.932 <0.001 食管胃底静脉曲张[例(%)] 16(18.39) 28(29.17) χ2=2.902 0.088 消化道出血[例(%)] 5(5.75) 15(15.63) χ2=4.575 0.032 腹水[例(%)] 15(17.24) 26(27.08) χ2=2.669 0.102 肝性脑病[例(%)] 2(2.30) 2(2.08) χ2=0.010 0.921 脾大[例(%)] 36(41.38) 46(47.92) χ2=0.789 0.374 脾功能亢进[例(%)] 25(28.74) 26(27.08) χ2=0.062 0.803 口干眼干[例(%)] 84(96.55) 10(10.42) χ2=135.540 <0.001 猖獗龋齿[例(%)] 37(42.53) 4(4.17) χ2=38.634 <0.001 腮腺肿大[例(%)] 30(34.48) 3(3.13) χ2=30.362 <0.001 肝硬化[例(%)] 35(40.23) 52(54.17) χ2=3.554 0.059 失代偿期肝硬化[例(%)] 33(37.93) 51(53.13) χ2=4.243 0.039 表 2 PBC合并SS组与单纯PBC组的自身阳性抗体比较
Table 2. Comparison of autoantibodies between Group PBC combined with SS and Group PBC-only
抗体 PBC合并SS
组(n=87)单纯PBC
组(n=96)χ2值 P值 ANA[例(%)] 87(100.00) 92(95.83) 3.706 0.054 SSA抗体[例(%)] 76(87.36) 6(6.25) 121.399 <0.001 SSB抗体[例(%)] 47(54.02) 2(2.08) 62.797 <0.001 CENP-B抗体[例(%)] 27(31.03) 20(20.83) 2.488 0.115 AMA-M2[例(%)] 79(90.80) 87(90.63) 0.002 0.967 SP100抗体[例(%)] 13(14.94) 19(19.79) 0.744 0.388 LKM1抗体[例(%)] 3(3.45) 2(2.08) 0.320 0.572 LC1抗体(例) 0 0 GP210抗体[例(%)] 19(21.84) 20(20.83) 0.028 0.868 SLA抗体[例(%)] 1(1.15) 0 1.110 0.292 注:ANA,抗核抗体;CENP-B抗体,抗着丝粒蛋白B抗体;AMA-M2,抗线粒体抗体M2型;SP100抗体,抗核点蛋白100抗体;LKM1抗体,抗肝肾微粒体抗体1型;LC1抗体,抗肝细胞溶质1型抗体;GP210抗体,抗核孔复合体糖蛋白210抗体;SLA抗体,抗可溶性肝抗原抗体。
表 3 PBC合并SS组与单纯PBC组的实验室指标比较
Table 3. Comparison of laboratory parameters between Group PBC combined with SS and Group PBC-only
指标 PBC合并SS组(n=87) 单纯PBC组(n=96) 统计值 P值 WBC(×109/L) 4.56(3.61~6.54) 4.74(3.36~6.85) Z=0.256 0.798 Hb(g/L) 113.00(103.00~127.00) 108.50(93.25~123.75) Z=2.106 0.035 PLT(×109/L) 138.00(87.00~198.00) 121.50(71.25~198.50) Z=0.954 0.340 LYM(×109/L) 1.27(0.80~1.84) 1.14(0.80~1.86) Z=0.407 0.684 NEUT(×109/L) 2.62(1.95~3.84) 2.94(2.07~4.22) Z=0.815 0.415 Alb(g/L) 37.90(31.20~41.40) 35.00(28.03~39.35) Z=2.571 0.010 ALT(U/L) 35.10(22.80~70.70) 56.15(28.43~100.00) Z=2.597 0.009 AST(U/L) 38.30(29.00~71.00) 68.30(41.98~98.76) Z=3.566 <0.001 ALP(U/L) 163.00(95.00~275.20) 207.45(155.48~368.00) Z=3.236 0.001 GGT(U/L) 140.20(79.00~326.70) 215.25(111.08~387.08) Z=2.027 0.043 TBil(U/L) 14.90(11.20~22.00) 32.90(16.43~85.80) Z=5.275 <0.001 CRE(U/L) 51.80(45.00~65.00) 53.25(45.00~67.00) Z=0.082 0.934 TG(U/L) 1.30(0.93~1.76) 1.28(0.87~1.86) Z=0.162 0.871 TC(U/L) 4.59(3.98~5.37) 4.84(3.42~6.59) Z=0.680 0.496 LDL(U/L) 2.52(1.88~3.08) 2.45(1.63~3.67) Z=0.604 0.546 ESR(mm/h) 28.00(15.00~49.00) 25.00(16.00~36.00) Z=1.054 0.292 CRP(mg/L) 3.80(2.49~5.98) 5.30(2.79~11.69) Z=2.447 0.014 PT(s) 11.90(11.10~13.50) 12.20(10.90~14.60) Z=1.063 0.288 INR 1.03(0.96~1.11) 1.05(0.94~1.27) Z=1.256 0.209 IgA(g/L) 3.02(2.14~3.99) 2.98(2.20~3.61) Z=0.590 0.555 IgG(g/L) 18.10(16.90~21.20) 13.50(11.40~16.88) Z=7.716 <0.001 IgM(g/L) 2.97(2.13~3.88) 3.15(2.72~5.46) Z=2.342 0.019 C3(g/L) 0.85±0.26 0.88±0.23 t=0.904 0.343 C4(g/L) 0.23(0.18~0.29) 0.23(0.16~0.27) Z=0.829 0.407 注:WBC,白细胞;PLT,血小板;LYM,淋巴细胞;NEUT,中性粒细胞;CRE,肌酐;TG,甘油三酯;TC,总胆固醇;LDL,低密度脂蛋白;ESR,血细胞沉降率;PT,凝血酶原时间;INR,国际标准化比率;C3,补体3;C4,补体4。
表 4 PBC患者合并SS的影响因素分析
Table 4. Regression analysis of potential influencing factors for concomitant SS diagnosis in patients with PBC
因素 B值 SE Wald P值 OR 95%CI 皮肤巩膜黄染 0.677 0.570 1.412 0.235 1.969 0.644~6.016 纳差 -0.952 0.499 3.640 0.056 0.386 0.145~1.026 消化道出血 -0.771 0.813 0.899 0.343 0.463 0.094~2.276 肝硬化失代偿 0.390 0.533 0.536 0.464 1.477 0.520~4.194 Hb(g/L) 0.009 0.013 0.431 0.511 1.099 0.950~1.235 ALT(U/L) -0.007 0.004 2.760 0.097 1.007 0.934~1.219 ALP(U/L) -0.001 0.002 0.366 0.545 0.935 0.900~1.219 AST(U/L) -0.004 0.005 0.597 0.440 0.996 0.939~1.398 GGT(U/L) -0.001 0.001 0.549 0.459 0.900 0.860~1.248 TBil(U/L) -0.020 0.007 8.026 0.005 0.760 0.700~0.811 Alb(g/L) 0.043 0.044 0.921 0.337 1.043 0.957~1.138 IgG(g/L) 0.470 0.081 33.444 <0.001 1.600 1.364~1.876 IgM(g/L) -0.096 0.147 0.430 0.512 0.908 0.681~1.211 表 5 PBC患者合并SS的两种预测模型的基本参数比较
Table 5. Comparison of key parameters between two predictive models for disease in patients with PBC with concomitant SS
模型 特异度 敏感度 AUC 95%CI 约登指数 MLR模型 0.875 0.759 0.896 0.843~0.936 0.633 6 ANN模型 0.875 0.839 0.919 0.870~0.954 0.714 1 -
[1] TRIVEDI PJ, HIRSCHFIELD GM, ADAMS DH, et al. Immunopathogenesis of primary biliary cholangitis, primary sclerosing cholangitis and autoimmune hepatitis: Themes and concepts[J]. Gastroenterology, 2024, 166( 6): 995- 1019. DOI: 10.1053/j.gastro.2024.01.049. [2] Chinese Society of Hepatology, Chinese Medical Association. Guidelines on the diagnosis and management of primary biliary cholangitis(2021)[J]. J Clin Hepatol, 2022, 38( 1): 35- 41.中华医学会肝病学分会. 原发性胆汁性胆管炎的诊断和治疗指南(2021)[J]. 临床肝胆病杂志, 2022, 38( 1): 35- 41. [3] SELMI C, ERIC GERSHWIN M. Chronic autoimmune epithelitis in Sjögren’s syndrome and primary biliary cholangitis: A comprehensive review[J]. Rheumatol Ther, 2017, 4( 2): 263- 279. DOI: 10.1007/s40744-017-0074-2. [4] EFE C, TORGUTALP M, HENRIKSSON I, et al. Extrahepatic autoimmune diseases in primary biliary cholangitis: Prevalence and significance for clinical presentation and disease outcome[J]. J Gastroenterol Hepatol, 2021, 36( 4): 936- 942. DOI: 10.1111/jgh.15214. [5] BAXT WG. Use of an artificial neural network for data analysis in clinical decision-making: The diagnosis of acute coronary occlusion[J]. Neural Comput, 1990, 2( 4): 480- 489. DOI: 10.1162/neco.1990.2.4.480. [6] LINDOR KD, GERSHWIN ME, POUPON R, et al. Primary biliary cirrhosis[J]. Hepatology, 2009, 50( 1): 291- 308. DOI: 10.1002/hep.22906. [7] VITALI C, BOMBARDIERI S, JONSSON R, et al. Classification criteria for Sjögren’s syndrome: A revised version of the European criteria proposed by the American-European consensus group[J]. Ann Rheum Dis, 2002, 61( 6): 554- 558. DOI: 10.1136/ard.61.6.554. [8] SANTOS GA, BRANDÃO M, FARINHA F. Prevalence of primary biliary cholangitis in a cohort of primary Sjögren’s syndrome patients[J]. Cureus, 2022, 14( 4): e24590. DOI: 10.7759/cureus.24590. [9] LIU ZC, WANG ZL, ZHENG JR, et al. Prevalence of primary biliary cholangitis in the Chinese general population and its influencing factors: A systematic review[J]. J Clin Hepatol, 2023, 39( 2): 325- 332. DOI: 10.3969/j.issn.1001-5256.2023.02.011.刘智成, 王资隆, 郑佳睿, 等. 我国一般人群原发性胆汁性胆管炎患病率及其影响因素的系统综述[J]. 临床肝胆病杂志, 2023, 39( 2): 325- 332. DOI: 10.3969/j.issn.1001-5256.2023.02.011. [10] WEN ZH, YAO FL, LING Q, et al. Similarities and differences between primary biliary cholangitis and Sjogren’s syndrome[J]. Med J Natl Defending Forces Southwest China, 2019, 29( 11): 1108- 1110. DOI: 10.3969/j.issn.1004-0188.2019.11.006.文振华, 姚芳玲, 凌青, 等. 原发性胆汁性胆管炎有无合并干燥综合征的异同[J]. 西南国防医药, 2019, 29( 11): 1108- 1110. DOI: 10.3969/j.issn.1004-0188.2019.11.006. [11] TRIVELLA J, JOHN BV, LEVY C. Primary biliary cholangitis: Epidemiology, prognosis, and treatment[J]. Hepatol Commun, 2023, 7( 6): e0179. DOI: 10.1097/HC9.0000000000000179. [12] JOHN BV, KHAKOO NS, SCHWARTZ KB, et al. Ursodeoxycholic acid response is associated with reduced mortality in primary biliary cholangitis with compensated cirrhosis[J]. Am J Gastroenterol, 2021, 116( 9): 1913- 1923. DOI: 10.14309/ajg.0000000000001280. [13] SUN Y, ZHANG WC, LI BS, et al. The coexistence of Sjögren’s syndrome and primary biliary cirrhosis: A comprehensive review[J]. Clin Rev Allergy Immunol, 2015, 48( 2-3): 301- 315. DOI: 10.1007/s12016-015-8471-1. [14] FLOREANI A, FRANCESCHET I, CAZZAGON N. Primary biliary cirrhosis: Overlaps with other autoimmune disorders[J]. Semin Liver Dis, 2014, 34( 3): 352- 360. DOI: 10.1055/s-0034-1383734. [15] LIU YW, HAN K, LIU C, et al. Clinical characteristics and prognosis of concomitant primary biliary cholangitis and autoimmune diseases: A retrospective study[J]. Can J Gastroenterol Hepatol, 2021, 2021: 5557814. DOI: 10.1155/2021/5557814. [16] WESIERSKA-GADEK J, PENNER E, BATTEZZATI PM, et al. Correlation of initial autoantibody profile and clinical outcome in primary biliary cirrhosis[J]. Hepatology, 2006, 43( 5): 1135- 1144. DOI: 10.1002/hep.21172. [17] LIU ZY, XU LS, LIU B. Detection of anti-kelch-like 12 and anti-hexokinase 1 antibodies in primary biliary cholangitis patients in China[J]. Rev Esp Enferm Dig, 2021, 113( 8): 585- 590. DOI: 10.17235/reed.2020.7483/2020. [18] CORPECHOT C, CHAZOUILLÈRES O, POUPON R. Early primary biliary cirrhosis: Biochemical response to treatment and prediction of long-term outcome[J]. J Hepatol, 2011, 55( 6): 1361- 1367. DOI: 10.1016/j.jhep.2011.02.031. [19] CARBONE M, SHARP SJ, FLACK S, et al. The UK-PBC risk scores: Derivation and validation of a scoring system for long-term prediction of end-stage liver disease in primary biliary cholangitis[J]. Hepatology, 2016, 63( 3): 930- 950. DOI: 10.1002/hep.28017. [20] TAKANO K, SAEKI C, OIKAWA T, et al. IgM response is a prognostic biomarker of primary biliary cholangitis treated with ursodeoxycholic acid and bezafibrate[J]. J Gastroenterol Hepatol, 2020, 35( 4): 663- 672. DOI: 10.1111/jgh.14900. [21] MAŚLIŃSKA M, WOJCIECHOWSKA B, MAŃCZAK M, et al. Serum immunoglobulin G4 in Sjögren’s syndrome: A pilot study[J]. Rheumatol Int, 2020, 40( 4): 555- 561. DOI: 10.1007/s00296-020-04529-0. [22] TEGLIA CM, GUIÑEZ M, GOICOECHEA HC, et al. Enhancement of multianalyte mass spectrometry detection through response surface optimization by least squares and artificial neural network modelling[J]. J Chromatogr A, 2020, 1611: 460613. DOI: 10.1016/j.chroma.2019.460613. -



 PDF下载 ( 1162 KB)
PDF下载 ( 1162 KB)

 下载:
下载:



