中药逆转肝纤维化的分子机制
DOI: 10.12449/JCH250126
利益冲突声明:本文不存在任何利益冲突。
作者贡献声明:郭晓玲负责文献检索,撰写论文;张静负责拟定文章思路;贾战生负责指导及最终定稿。
-
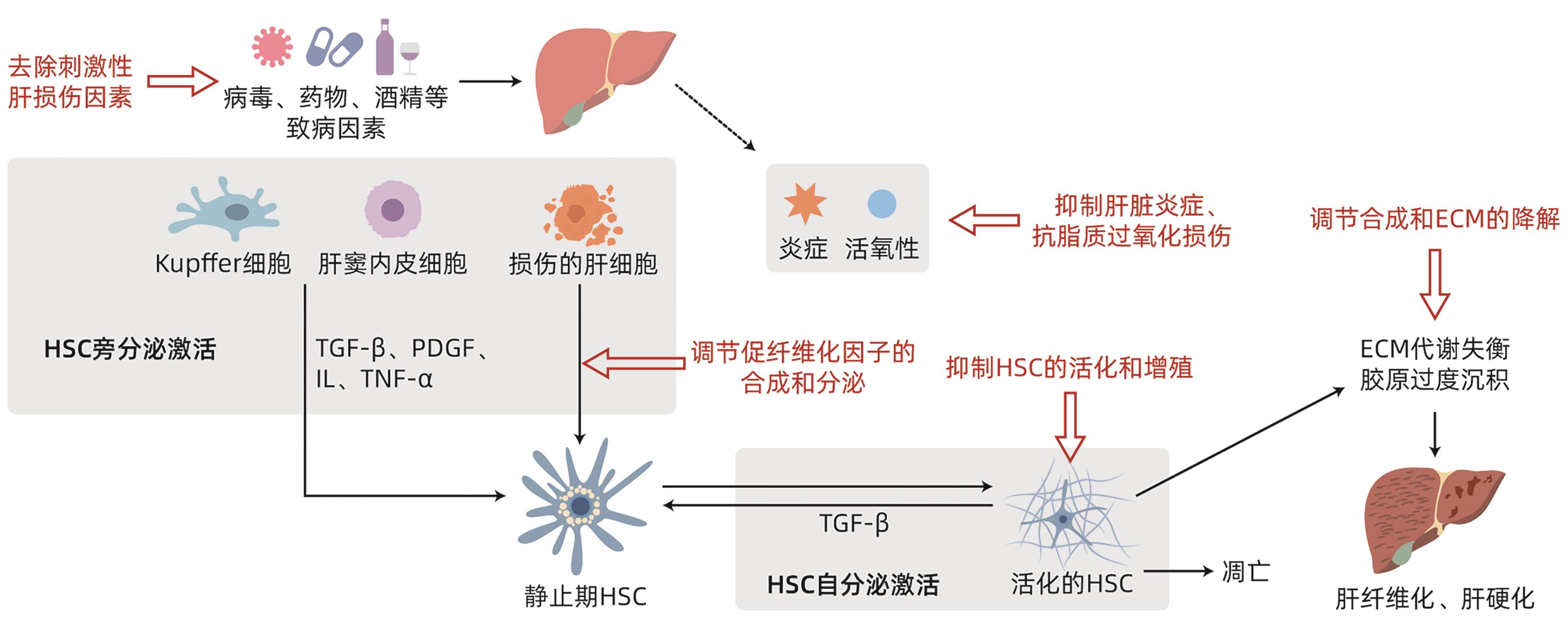
摘要: 肝纤维化是许多慢性肝病进展为肝硬化的中间环节,虽然目前尚未研发出能被广泛接受和有效的化学或生物制剂来逆转肝纤维化,但其在中药治疗方面已取得了巨大的进步。本文对不同草药提取物、单味中药、中成药逆转肝纤维化的分子机制进行了阐述,包括抑制肝脏炎症、抗脂质过氧化损伤、抑制肝星状细胞活化和增殖、调节促纤维化因子的合成和分泌、调节合成和细胞外基质的降解等5个方面,以期为未来治疗肝纤维化提供更精准的选择。
-
关键词:
- 肝纤维化 /
- 抗肝纤维化药(中药) /
- 药理作用分子作用机制
Abstract: Liver fibrosis is the intermediate stage in the progression of many chronic liver diseases to liver cirrhosis, and although there is still a lack of widely accepted and effective chemical or biological agents for reversing liver fibrosis, significant progress has been made in the treatment of liver fibrosis with traditional Chinese medicine. This article elaborates on the molecular mechanisms of different herbal extracts, a single Chinese herb, and Chinese patent drugs in reversing liver fibrosis, such as inhibiting liver inflammation, exerting an effect on lipid peroxidation damage, inhibiting the activation and proliferation of hepatic stellate cells, regulating the synthesis and secretion of pro-fibrogenic factors, and regulating the synthesis and degradation of extracellular matrix, in order to provide more precise options for the treatment of liver fibrosis in the future. -
[1] CHANG ML, YANG SS. Metabolic signature of hepatic fibrosis: From individual pathways to systems biology[J]. Cells, 2019, 8( 11): 1423. DOI: 10.3390/cells8111423. [2] Liver Disease Committee, Chinese Association of Integrative Medicine. Guidelines for the diagnosis and treatment of liver fibrosis in integrative medicine practice(2019)[J]. J Clin Hepatol, 2019, 35( 7): 1444- 1449. DOI: 10.3969/j.issn.1001-5256.2019.07.007.中国中西医结合学会肝病专业委员会. 肝纤维化中西医结合诊疗指南(2019年版)[J]. 临床肝胆病杂志, 2019, 35( 7): 1444- 1449. DOI: 10.3969/j.issn.1001-5256.2019.07.007. [3] LI YW, LU YR, NIAN MZ, et al. Therapeutic potential and mechanism of Chinese herbal medicines in treating fibrotic liver disease[J]. Chin J Nat Med, 2023, 21( 9): 643- 657. DOI: 10.1016/S1875-5364(23)60443-1. [4] DAWOOD RM, EL-MEGUID MA, SALUM GM, et al. Key players of hepatic fibrosis[J]. J Interferon Cytokine Res, 2020, 40( 10): 472- 489. DOI: 10.1089/jir.2020.0059. [5] KIM HY, SAKANE S, EGUILEOR A, et al. The origin and fate of liver myofibroblasts[J]. Cell Mol Gastroenterol Hepatol, 2024, 17( 1): 93- 106. DOI: 10.1016/j.jcmgh.2023.09.008. [6] DEL CAMPO JA, GALLEGO P, GRANDE L. Role of inflammatory response in liver diseases: Therapeutic strategies[J]. World J Hepatol, 2018, 10( 1): 1- 7. DOI: 10.4254/wjh.v10.i1.1. [7] SUN MX, KISSELEVA T. Reversibility of liver fibrosis[J]. Clin Res Hepatol Gastroenterol, 2015, 39( Suppl 1): S60- S63. DOI: 10.1016/j.clinre.2015.06.015. [8] SHAN L, LIU ZN, CI LL, et al. Research progress on the anti-hepatic fibrosis action and mechanism of natural products[J]. Int Immunopharmacol, 2019, 75: 105765. DOI: 10.1016/j.intimp.2019.105765. [9] KISSELEVA T, BRENNER D. Molecular and cellular mechanisms of liver fibrosis and its regression[J]. Nat Rev Gastroenterol Hepatol, 2021, 18( 3): 151- 166. DOI: 10.1038/s41575-020-00372-7. [10] SIMBRUNNER B, VILLESEN IF, KÖNIGSHOFER P, et al. Systemic inflammation is linked to liver fibrogenesis in patients with advanced chronic liver disease[J]. Liver Int, 2022, 42( 11): 2501- 2512. DOI: 10.1111/liv.15365. [11] ZHAO HW, ZHANG ZF, CHAI X, et al. Oxymatrine attenuates CCl4-induced hepatic fibrosis via modulation of TLR4-dependent inflammatory and TGF-β1 signaling pathways[J]. Int Immunopharmacol, 2016, 36: 249- 255. DOI: 10.1016/j.intimp.2016.04.040. [12] ZHANG JB, JIN HL, FENG XY, et al. The combination of Lonicerae Japonicae Flos and Forsythiae Fructus herb-pair alleviated inflammation in liver fibrosis[J]. Front Pharmacol, 2022, 13: 984611. DOI: 10.3389/fphar.2022.984611. [13] SHANG X, YUAN H, DAI L, et al. Anti-liver fibrosis activity and the potential mode of action of Ruangan Granules: Integrated network pharmacology and metabolomics[J]. Front Pharmacol, 2021, 12: 754807. DOI: 10.3389/fphar.2021.754807. [14] KIM HY, CHOI YJ, KIM SK, et al. Auranofin prevents liver fibrosis by system Xc-mediated inhibition of NLRP3 inflammasome[J]. Commun Biol, 2021, 4( 1): 824. DOI: 10.1038/s42003-021-02345-1. [15] WANG XM, CUI YQ, WANG J, et al. Liuwei Dihuang pills attenuates liver fibrosis by inhibiting macrophage activation in CCl4 induced liver injury[J]. J Nanjing Univ Tradit Chin Med, 2017, 33( 1): 65- 68. DOI: 10.14148/j.issn.1672-0482.2016.0065.王学敏, 崔亚钦, 王静, 等. 六味地黄丸抑制巨噬细胞激活抗肝纤维化作用机制研究[J]. 南京中医药大学学报, 2017, 33( 1): 65- 68. DOI: 10.14148/j.issn.1672-0482.2016.0065. [16] LI Z, ZHU JF, OUYANG H. Progress on traditional Chinese medicine in improving hepatic fibrosis through inhibiting oxidative stress[J]. World J Hepatol, 2023, 15( 10): 1091- 1108. DOI: 10.4254/wjh.v15.i10.1091. [17] YU HY, JIANG X, DONG FY, et al. Lipid accumulation-induced hepatocyte senescence regulates the activation of hepatic stellate cells through the Nrf2-antioxidant response element pathway[J]. Exp Cell Res, 2021, 405( 2): 112689. DOI: 10.1016/j.yexcr.2021.112689. [18] DHAR D, BAGLIERI J, KISSELEVA T, et al. Mechanisms of liver fibrosis and its role in liver cancer[J]. Exp Biol Med(Maywood), 2020, 245( 2): 96- 108. DOI: 10.1177/1535370219898141. [19] KONG R, WANG N, LUO H, et al. Hesperetin Mitigates bile duct ligation-induced liver fibrosis by inhibiting extracellular matrix and cell apoptosis via the TGF-β1/Smad pathway[J]. Curr Mol Med, 2018, 18( 1): 15- 24. DOI: 10.2174/1566524018666180608084947. [20] MIAO Y, WU YL, JIN YJ, et al. Benzoquinone derivatives with antioxidant activity inhibit activated hepatic stellate cells and attenuate liver fibrosis in TAA-induced mice[J]. Chem Biol Interact, 2020, 317: 108945. DOI: 10.1016/j.cbi.2020.108945. [21] WU TH, WANG PW, LIN TY, et al. Antioxidant properties of red raspberry extract alleviate hepatic fibrosis via inducing apoptosis and transdifferentiation of activated hepatic stellate cells[J]. Biomed Pharmacother, 2021, 144: 112284. DOI: 10.1016/j.biopha.2021.112284. [22] GUO YJ, LIANG XM, MENG MY, et al. Hepatoprotective effects of Yulangsan flavone against carbon tetrachloride(CCl4)-induced hepatic fibrosis in rats[J]. Phytomedicine, 2017, 33: 28- 35. DOI: 10.1016/j.phymed.2017.07.005. [23] JANGRA A, KOTHARI A, SARMA P, et al. Recent advancements in antifibrotic therapies for regression of liver fibrosis[J]. Cells, 2022, 11( 9): 1500. DOI: 10.3390/cells11091500. [24] WANG Q, DAI XF, YANG WZ, et al. Caffeine protects against alcohol-induced liver fibrosis by dampening the cAMP/PKA/CREB pathway in rat hepatic stellate cells[J]. Int Immunopharmacol, 2015, 25( 2): 340- 352. DOI: 10.1016/j.intimp.2015.02.012. [25] BAI FC, HUANG QF, NIE JL, et al. Trolline ameliorates liver fibrosis by inhibiting the NF-κB pathway, promoting HSC apoptosis and suppressing autophagy[J]. Cell Physiol Biochem, 2017, 44( 2): 436- 446. DOI: 10.1159/000485009. [26] WANG JH, GUO XH, ZHENG BW, et al. Mechanism of curcumol against liver fibrosis based on miR-125b/NLRP3 signaling pathway[J]. Chin Arch Tradit Chin Med, 2022, 40( 11): 95- 99. DOI: 10.13193/j.issn.1673-7717.2022.11.023.王佳慧, 郭新华, 郑博文, 等. 基于miR-125b/NLRP3信号通路探讨莪术醇抗肝纤维化的作用机制[J]. 中华中医药学刊, 2022, 40( 11): 95- 99. DOI: 10.13193/j.issn.1673-7717.2022.11.023. [27] XING XR. Multi-target based mechansim investigation of Fuzheng Huayu Formula in treating liver fibrosis[D]. Shanghai: Naval Medical University, 2019.邢心睿. 扶正化瘀方抗肝纤维化的网络多靶标作用机制研究[D]. 上海: 中国人民解放军海军军医大学, 2019. [28] SUN X, PING DB, PENG Y, et al. Fuzheng Huayu Fang enhances the anti-liver fibrosis mechanism of action of NK cells to kill and activate liver stellate cells[C]// Proceedings of the Thirteenth National Academic Conference on Integrated Traditional Chinese Medicine and Western Medicine for Digestive System Diseases. 2019: 274- 275. DOI: 10.26914/c.cnkihy.2019.016545.孙鑫, 平大冰, 彭渊, 等. 扶正化瘀方通过增强NK细胞杀伤活化肝星状细胞的抗肝纤维化作用机制[C]// 第三十一届全国中西医结合消化系统疾病学术会议论文集. 2019: 274- 275. DOI: 10.26914/c.cnkihy.2019.016545. [29] ACHARYA P, CHOUHAN K, WEISKIRCHEN S, et al. Cellular mechanisms of liver fibrosis[J]. Front Pharmacol, 2021, 12: 671640. DOI: 10.3389/fphar.2021.671640. [30] LIN YC, LUO HY, WANG X, et al. Flavanones from Sedum sarmentosum bunge alleviate CCl4-induced liver fibrosis in rats by targeting TGF-β1/TβR/smad pathway in turn inhibiting epithelial mesenchymal transition[J]. Evid Based Complement Alternat Med, 2018, 2018: 3080837. DOI: 10.1155/2018/3080837. [31] ZHANG GK, JIANG YY, LIU X, et al. Lingonberry anthocyanins inhibit hepatic stellate cell activation and liver fibrosis via TGFβ/smad/ERK signaling pathway[J]. J Agric Food Chem, 2021, 69( 45): 13546- 13556. DOI: 10.1021/acs.jafc.1c05384. [32] SHENG JP, ZHANG BH, CHEN YF, et al. Capsaicin attenuates liver fibrosis by targeting Notch signaling to inhibit TNF-α secretion from M1 macrophages[J]. Immunopharmacol Immunotoxicol, 2020, 42( 6): 556- 563. DOI: 10.1080/08923973.2020.1811308. [33] HUANG Y, XIA L, LEI QS, et al. Protective effects and mechanism of saikosaponin D on immune hepatic fibrosis in rats[J]. J Army Med Univ, 2022, 44( 14): 1410- 1420. DOI: 10.16016/j.2097-0927.202111062.黄祎, 夏莉, 雷青松, 等. 柴胡皂苷D对大鼠免疫性肝纤维化的保护作用及其机制研究[J]. 陆军军医大学学报, 2022, 44( 14): 1410- 1420. DOI: 10.16016/j.2097-0927.202111062. [34] KHURANA A, SAYED N, ALLAWADHI P, et al. It’s all about the spaces between cells: Role of extracellular matrix in liver fibrosis[J]. Ann Transl Med, 2021, 9( 8): 728. DOI: 10.21037/atm-20-2948. [35] MENGGENSILIMU, YUAN HW, ZHAO CM, et al. Anti-liver fibrosis effect of total flavonoids from Scabiosa comosa Fisch. ex Roem. et Schult. on liver fibrosis in rat models and its proteomics analysis[J]. Ann Palliat Med, 2020, 9( 2): 272- 285. DOI: 10.21037/apm.2020.02.29. [36] LI Q, WU HC, TAN JX, et al. Study on machanism of Rougan Formula in anti-hepatic fibrosis by inhibiting fibrosin[J]. Chin J Immunol, 2022, 38( 3): 263- 269. DOI: 10.3969/j.issn.1000-484X.2022.03.002.李茜, 吴惠春, 谭家鑫, 等. 柔肝方通过抑制纤维化蛋白抗肝纤维化的机制研究[J]. 中国免疫学杂志, 2022, 38( 3): 263- 269. DOI: 10.3969/j.issn.1000-484X.2022.03.002. [37] LI ZB, JIANG L, NI JD, et al. Salvianolic acid B suppresses hepatic fibrosis by inhibiting ceramide glucosyltransferase in hepatic stellate cells[J]. Acta Pharmacol Sin, 2023, 44( 6): 1191- 1205. DOI: 10.1038/s41401-022-01044-9. [38] WU HY, GU YQ, ZHOU HC, et al. Effects of cycloastragenol on carbon tetrachloride-induced hepatic fibrosis and glycolysis in mice[J]. China Pharm, 2022, 33( 14): 1677- 1681, 1687. DOI: 10.6039/j.issn.1001-0408.2022.14.03.吴红雁, 顾亚琴, 周红成, 等. 环黄芪醇对四氯化碳致小鼠肝纤维化及糖酵解的影响[J]. 中国药房, 2022, 33( 14): 1677- 1681, 1687. DOI: 10.6039/j.issn.1001-0408.2022.14.03. [39] GUO T, LIU ZL, ZHAO Q, et al. A combination of astragaloside I, levistilide A and calycosin exerts anti-liver fibrosis effects in vitro and in vivo[J]. Acta Pharmacol Sin, 2018, 39( 9): 1483- 1492. DOI: 10.1038/aps.2017.175. [40] SUN X, TAN Y, LYU J, et al. Active components formulation developed from Fuzheng Huayu Recipe for anti-liver fibrosis[J]. Chin J Integr Med, 2022, 28( 6): 538- 544. DOI: 10.1007/s11655-021-3293-x. -



 PDF下载 ( 917 KB)
PDF下载 ( 917 KB)

 下载:
下载:


