人工肝治疗肝衰竭患者血红蛋白水平的变化及其影响因素
DOI: 10.12449/JCH250116
Changes in hemoglobin and related influencing factors in patients with liver failure undergoing artificial liver support therapy
-
摘要:
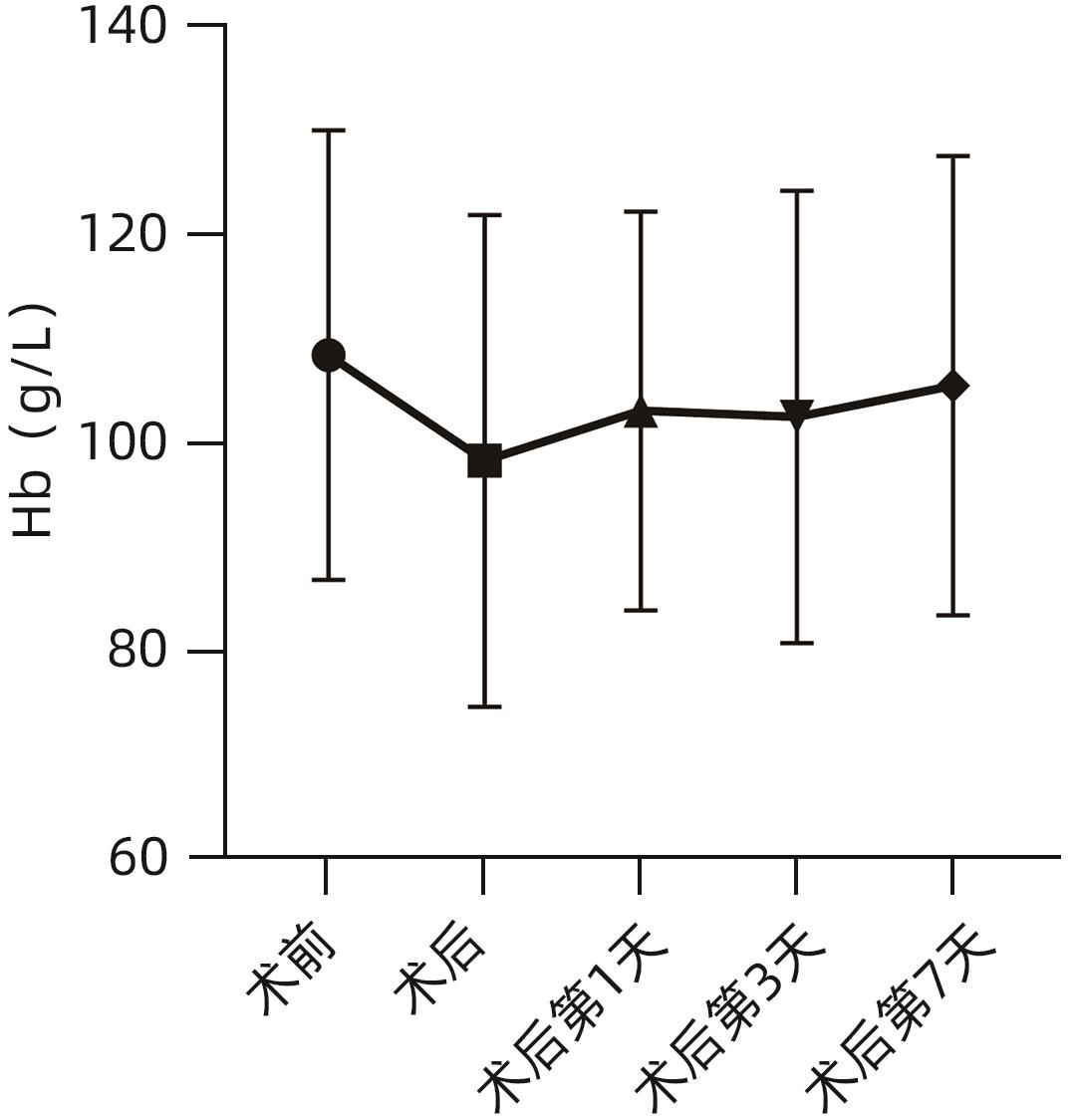
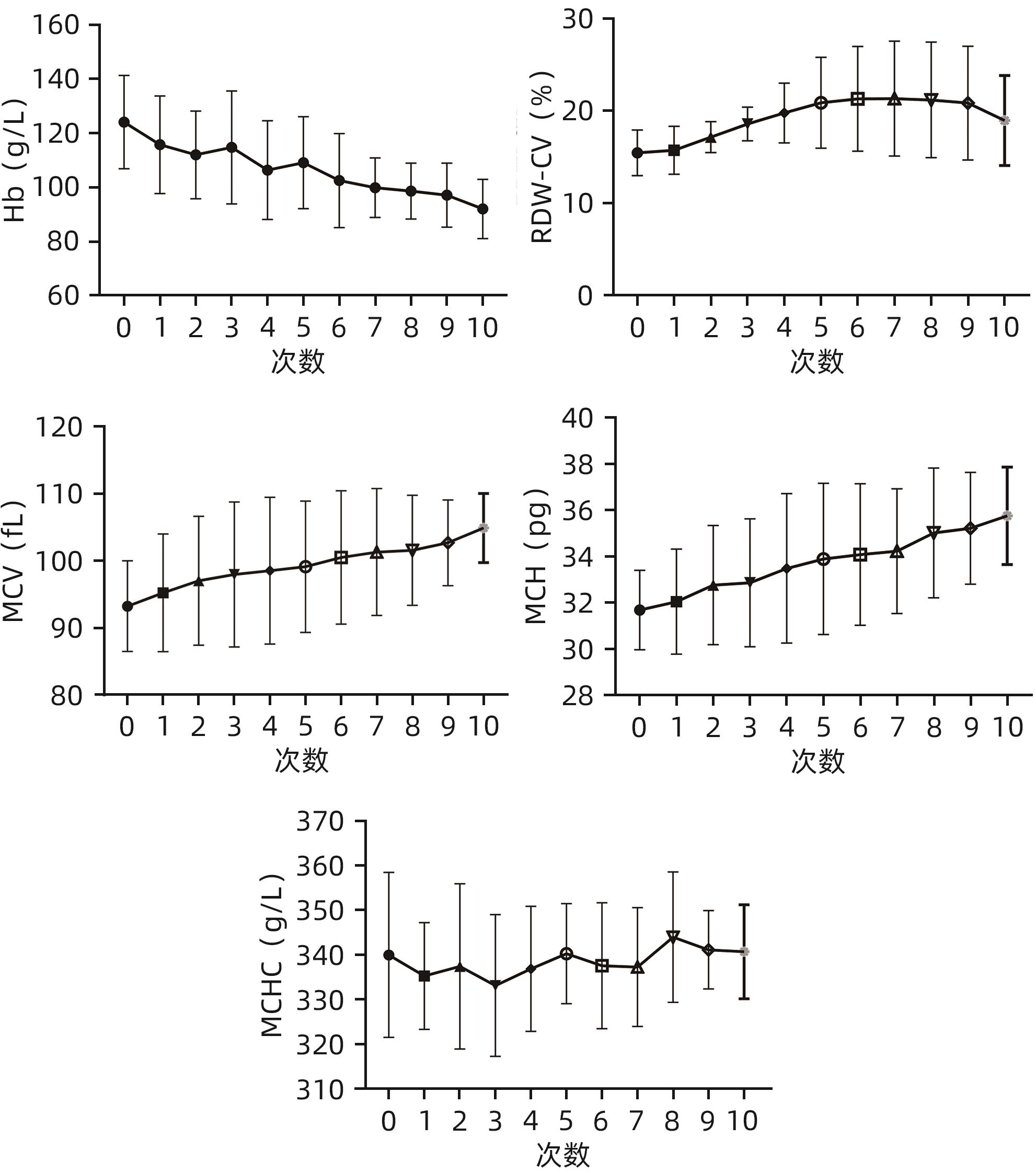
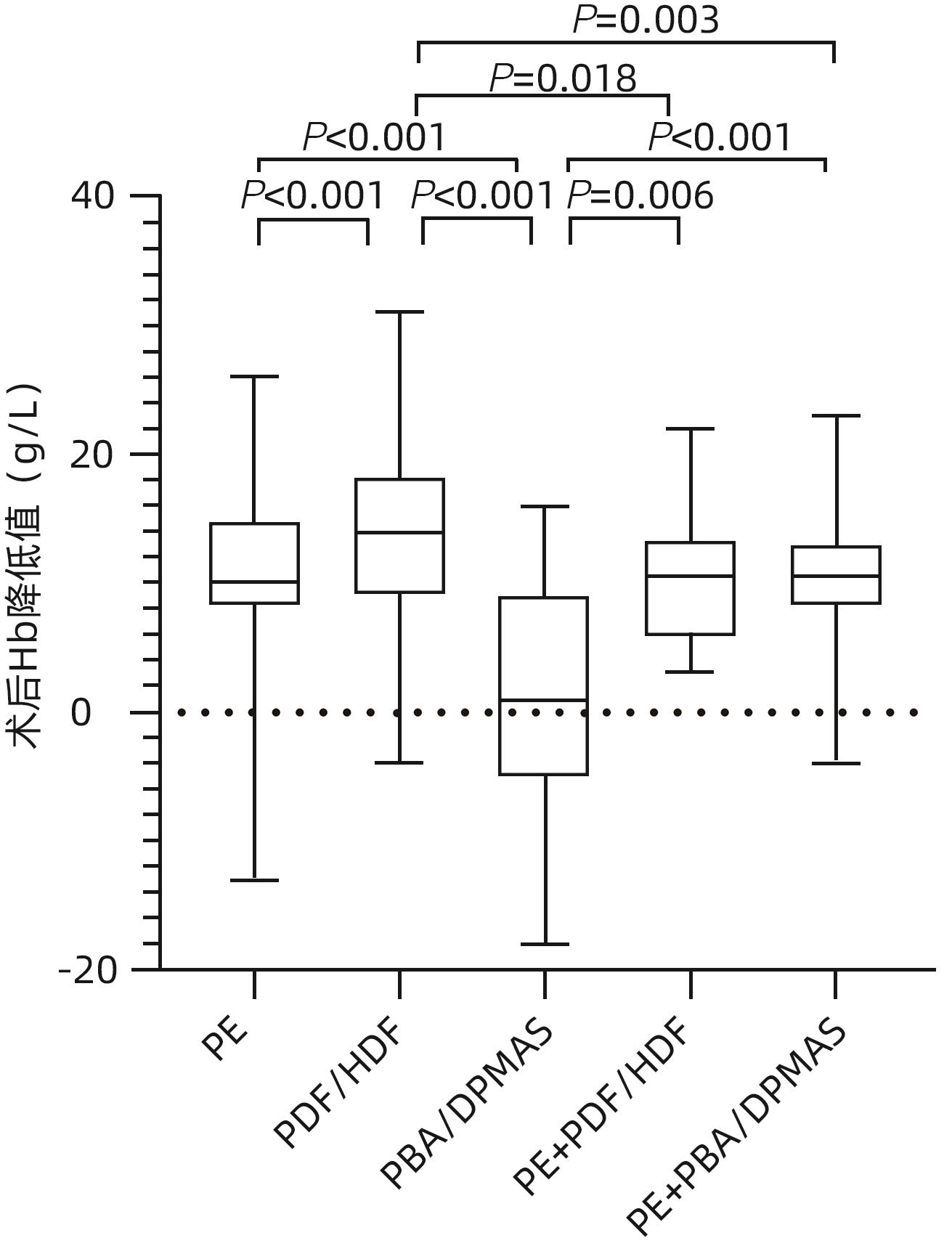
目的 探讨肝衰竭患者接受人工肝治疗后血红蛋白(Hb)变化趋势和影响因素。 方法 选取2018年1月—12月在福建医科大学孟超肝胆医院接受人工肝治疗的肝衰竭患者106例,分析患者的临床资料与Hb、平均红细胞体积(MCV)、平均红细胞血红蛋白含量(MCH)、平均红细胞血红蛋白浓度(MCHC)和红细胞分布宽度变异系数(RDW-CV)等红细胞参数。重复测量资料组间比较采用单因素重复测量方差分析,两两比较采用配对t检验;偏态分布的计量资料多组间比较采用Kruskal-Wallis H检验,两两比较采用Mann-Whitney U检验。采用单因素及多因素线性回归分析人工肝治疗后Hb降低的影响因素。 结果 106例肝衰竭患者接受606人次人工肝治疗,其中402人次治疗前后均有Hb检测结果,肝衰竭患者接受人工肝治疗术后Hb[(97.49±20.51)g/L]较术前[(109.38±20.22)g/L]下降(t=32.764,P<0.001)。进一步对14例肝衰竭患者纵向观察,末次人工肝治疗术前Hb为(108.50±21.61)g/L,术后次日Hb[(103.14±19.15)g/L]较前恢复,术后第3天Hb[(102.57±21.73)g/L]未进一步回升,术后第7天Hb再次升高[(105.57±22.04)g/L]。肝衰竭患者术后次日Hb水平随着治疗次数的增加而降低(F=8.996,P<0.001),而MCV和MCH随着治疗次数的增加逐渐增高(F值分别为9.154和13.460,P值分别为0.004和<0.001),RDW-CV则先逐渐升高后下降(F=4.520,P=0.032),MCHC呈上下波动,无明显趋势(F=0.811,P=0.494)。多因素线性回归分析显示,人工肝操作时长、模式和首次治疗是人工肝治疗后Hb减少的独立危险因素(P值均<0.05)。 结论 人工肝治疗可影响肝衰竭患者外周Hb水平,应加强肝衰竭人工肝治疗期间的患者血液管理。 Abstract:Objective To investigate the changing trend of hemoglobin (Hb) and related influencing factors in patients with liver failure after artificial liver support system (ALSS) therapy. Methods A total of 106 patients with liver failure who were hospitalized and received ALSS therapy in our hospital from January to December 2018 were enrolled and analyzed in terms of clinical data and red blood cell parameters such as Hb, mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), and red blood cell distribution width-coefficient of variation (RDW-CV). A one-way repeated-measures analysis of variance was used for comparison of continuous data with repeated measurement between groups, and the paired t-test was used for comparison between two groups. The Kruskal-Wallis H test was used for comparison of continuous data with skewed distribution between multiple groups, the Mann-Whitney U test was used for further comparison between two groups. Univariate and multivariate linear regression analyses were used to identify the influencing factors for the reduction in Hb after ALSS therapy. Results The 106 patients with liver failure received 606 sessions of ALSS therapy, and Hb was measured for 402 sessions before and after treatment. There was a significant reduction in Hb after ALSS therapy in the patients with liver failure (97.49±20.51 g/L vs 109.38±20.22 g/L, t=32.764, P<0.001). Longitudinal observation was further performed for 14 patients with liver failure, and the results showed that the level of Hb was 108.50±21.61 g/L before the last session of ALSS therapy, with certain recovery compared with the level of Hb (103.14±19.15 g/L) on the second day after ALSS, and there was an increase in Hb on day 3 (102.57±21.73 g/L) and day 7 (105.57±22.04 g/L) after surgery. The level of Hb in patients with liver failure on the second day after ALSS decreased with the increase in the number of ALSS sessions (F=8.996, P<0.001), while MCV and MCH gradually increased with the increase in the number of ALSS sessions (F=9.154 and 13.460, P=0.004 and P<0.001), and RDW-CV first gradually increased and then gradually decreased (F=4.520, P=0.032); MCHC showed fluctuations with no clear trend (F=0.811, P=0.494). The multivariate linear regression analysis showed that the duration of ALSS therapy, the mode of ALSS therapy, and initial treatment were independent risk factors for the reduction in Hb after ALSS therapy. Conclusion ALSS therapy can influence the level of peripheral blood Hb in patients with liver failure, and patient blood management should be strengthened for patients with liver failure who are receiving ALSS therapy. -
Key words:
- Liver Failure /
- Liver, Artificial /
- Hemoglobins
-
表 1 肝衰竭患者人工肝治疗前的基本临床和实验室资料
Table 1. Clinical and laboratory data before artificial liver therapy in patients with liver failure
指标 数值 年龄(岁) 46(37~55) 性别[例(%)] 男 89(83.96) 女 17(16.04) 肝衰竭类型[例(%)] 亚急性肝衰竭 6(5.66) 慢加急性(亚急性)肝衰竭 93(87.74) 慢性肝衰竭 7(6.60) 肝衰竭分期[例(%)] 早期 9(8.49) 中期 63(59.43) 晚期 34(32.08) 肝衰竭病因[例(%)] 肝炎病毒 95(89.62) 药物性 3(2.83) 酒精性 1(0.94) 原因不明 7(6.60) 人工肝治疗次数[例(%)] ≤2次 15(14.15) 3次 17(16.04) 4次 10(9.43) 5次 14(13.21) 6次 12(11.32) 7次 14(13.21) ≥8次 24(22.64) 腹水(无/有) 55/51 肝性脑病分期(0/1/2/3/4) 85/11/6/2/2 身高(cm) 167.27±7.25 体质量(kg) 65(59~74) BMI(kg/m2) 23.54±3.33 血容量(mL) 4 408±552 MELD评分(分) 25.27±5.86 TBil(μmol) 373.2(333.5~464.0) Alb(g/L) 32.04±4.87 ALT(U/L) 323(113~665) AST(U/L) 225(111~498) Cr(μmol/L) 66(60~80) Amon(μmol/L) 58(44~83) PT(s) 24.4(20.7~31.3) INR 2.20(1.70~2.98) Hb(g/L) 123.64±21.34 表 2 8例肝衰竭患者10次人工肝术后次日红细胞参数值
Table 2. Red blood cell parameters on the day after 10 artificial liver therapy in 8 patients with liver failure
次数 Hb(g/L) RDW-CV(%) MCV(fL) MCH(pg) MCHC(g/L) 首次术前 124.13±17.27 15.49±2.48 93.26±6.76 31.69±1.72 340.38±17.25 1次 115.75±18.03 15.76±2.61 95.25±8.77 32.05±2.27 337.25±11.32 2次 112.00±16.20 17.19±1.67 97.05±9.59 32.76±2.58 338.63±17.11 3次 114.75±20.89 18.61±1.81 97.99±10.80 32.86±2.77 336.25±15.71 4次 106.38±18.29 19.80±3.24 98.55±10.93 33.49±3.24 339.38±13.53 5次 109.13±17.02 20.91±4.92 99.14±9.78 33.90±3.28 342.13±10.56 6次 102.50±17.37 21.34±5.68 100.51±9.94 34.09±3.06 339.50±13.24 7次 99.88±11.00 21.36±6.23 101.33±9.45 34.24±2.70 338.63±12.32 8次 98.63±10.36 21.23±6.25 101.59±8.20 35.03±2.81 345.13±13.52 9次 97.13±11.83 20.88±6.17 102.70±6.40 35.23±2.42 343.13±8.46 10次 92.00±10.94 18.99±4.87 104.90±5.15 35.76±2.11 341.00±10.03 F值 8.996 4.520 9.154 13.460 0.811 P值 <0.001 0.032 0.004 <0.001 0.494 表 3 人工肝治疗后Hb降低的影响因素分析
Table 3. Analysis of risk factors affecting Hb reduction after artificial liver therapy
参数 单因素线性回归分析 多因素线性回归分析 B值 SE β值 t值 P值 β值 t值 P值 年龄 0.045 0.028 0.081 1.634 0.103 性别 -0.025 0.400 -0.003 -0.062 0.950 身高 -0.014 0.053 -0.014 -0.269 0.788 体质量 -0.078 0.035 -0.114 -2.246 0.025 -0.101 -1.015 0.311 BMI -0.276 0.111 -0.125 -2.477 0.014 -0.015 -0.148 0.883 血容量 -0.001 0.001 -0.065 -1.305 0.193 肝衰竭类型 -0.124 0.967 -0.006 -0.128 0.898 肝衰竭分期 0.787 0.653 0.060 1.205 0.229 肝衰竭病因 0.881 0.493 0.089 1.788 0.075 0.057 -1.143 0.254 MELD评分 0.047 0.064 0.036 0.723 0.470 腹水 -0.033 0.325 -0.005 -0.102 0.919 肝性脑病 -0.198 0.338 -0.029 -0.584 0.560 人工肝治疗时长 0.009 0.004 0.105 2.119 0.035 0.189 3.374 0.001 人工肝模式 -0.604 0.289 -0.104 -2.087 0.038 -0.158 -2.841 0.005 人工肝次数 -0.387 0.119 -0.161 -3.256 0.001 -0.047 -0.825 0.410 首次人工肝 3.653 0.930 0.193 3.928 <0.001 0.157 2.768 0.006 -
[1] Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Associtaion; Severe Liver Disease and artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure(2018)[J]. J Clin Hepatol, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007.中华医学会感染病学分会肝衰竭与人工肝学组, 中华医学会肝病学分会重型肝病与人工肝学组 肝衰竭诊治指南(2018年版)[J]. 临床肝胆病杂志, 2019, 35( 1): 38- 44. DOI: 10.3969/j.issn.1001-5256.2019.01.007. [2] Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Expert consensus on clinical application of artificial liver and blood purification(2022 edition)[J]. J Clin Hepatol, 2022, 38( 5): 767- 775. DOI: 10.3969/j.issn.1001-5256.2022.04.007.中华医学会肝病学分会重型肝病与人工肝学组 人工肝血液净化技术临床应用专家共识(2022年版)[J]. 临床肝胆病杂志, 2022, 38( 4): 767- 775. DOI: 10.3969/j.issn.1001-5256.2022.04.007. [3] CAI YF, WANG ZH, CHENG SQ. A comparative study of three non-biological artificial liver models in the treatment of patients with acute-on-chronic liver failure[J/CD]. Chin J Liver Dis(Electronic Version), 2023, 15( 1): 47- 55. DOI: 10.3969/j.issn.1674-7380.2023.01.008.蔡毅峰, 王朝辉, 程书权. 三种非生物型人工肝模式治疗慢加急性肝衰竭患者的对比研究[J/CD]. 中国肝脏病杂志(电子版), 2023, 15( 1): 47- 55. DOI: 10.3969/j.issn.1674-7380.2023.01.008. [4] ZHANG B, DILIHUMAER ZYE, ZHANG SY, et al. Progress on pathogenesis and medical treatment of hepatitis B virus-related chronic and acute liver failure[J/CD]. Chin J Liver Dis(Electronic Version), 2023, 15( 1): 28- 33. DOI: 10.3969/j.issn.1674-7380.2023.01.005.张斌, 迪丽胡玛尔·扎依尔, 张诗雨, 等. 乙型肝炎相关慢加急性肝衰竭发病机制及治疗进展[J/CD]. 中国肝脏病杂志(电子版), 2023, 15( 1): 28- 33. DOI: 10.3969/j.issn.1674-7380.2023.01.005. [5] WANG L, XU WX, ZHU S, et al. Influence of artificial liver support system therapy on platelet in treatment of hepatitis B virus-related acute-on-chronic liver failure[J]. J Clin Hepatol, 2022, 38( 5): 1053- 1058. DOI: 10.3969/j.issn.1001-5256.2022.05.015.王璐, 许文雄, 朱姝, 等. 人工肝治疗HBV相关慢加急性肝衰竭的血小板计数变化及其影响因素[J]. 临床肝胆病杂志, 2022, 38( 5): 1053- 1058. DOI: 10.3969/j.issn.1001-5256.2022.05.015. [6] ZHU MF, HUANG JR, CHEN YM. Treatment with artificial liver support system-plaxma exchange blood cell in the patients of severe hippatitis[J]. Chin J Dial Artif Organs, 2004, 15( 1): 12- 15.朱梦飞, 黄建荣, 陈月美. 人工肝支持系统治疗对慢性重型肝炎患者近期血细胞影响的研究[J]. 透析与人工器官, 2004, 15( 1): 12- 15. [7] ZHANG K, XIE XS, YING YZ. The effect of plasma exchange on recent blood cells in patients with severe hepatitis[J]. Zhejiang Pract Med, 2006, 11( 5): 331, 336. DOI: 10.3969/j.issn.1007-3299.2006.05.017.张戡, 谢新生, 应雅珍. 血浆置换对重型肝炎患者近期血细胞的影响[J]. 浙江实用医学, 2006, 11( 5): 331, 336. DOI: 10.3969/j.issn.1007-3299.2006.05.017. [8] JIA JF, LIANG F, HUANG J, et al. Effect of artificial liver with double plasma molecular absorb system model on patients’ platelets and corresponding treatment strategy[J]. J Peking Univ: Health Sci, 2022, 54( 3): 548- 551. DOI: 10.19723/j.issn.1671-167X.2022.03.022.贾金凤, 梁菲, 黄建, 等 双重血浆分子吸附系统模式人工肝治疗对血小板的影响[J]. 北京大学学报(医学版), 2022, 54( 3): 548- 551. DOI: 10.19723/j.issn.1671-167X.2022.03.022. [9] WU YS, ZHANG H, ZHENG WH, et al. Hidden blood loss and the influential factors after percutaneous kyphoplasty surgery[J]. Eur Spine J, 2017, 26( 7): 1878- 1883. DOI: 10.1007/s00586-017-4950-9. [10] KAMATH PS, KIM WR, Advanced Liver Disease Study Group. The model for end-stage liver disease(MELD)[J]. Hepatology, 2007, 45( 3): 797- 805. DOI: 10.1002/hep.21563. [11] NIE C, SHE GM, LI YL, et al. Effect of cardiopulmonary bypass for 30 min on structure and mechanical properties of erythrocyte membrane surface[J]. Chin J Pathophysiol, 2015, 31( 9): 1611- 1616. DOI: 10.3969/j.issn.1000-4718.2015.09.014.聂偲, 佘高明, 李雅兰, 等. 体外循环30 min对红细胞膜的表面结构及力学特性的影响[J]. 中国病理生理杂志, 2015, 31( 9): 1611- 1616. DOI: 10.3969/j.issn.1000-4718.2015.09.014. [12] TANG JF, LU AW, ZHU HM, et al. Application of blood cell multi-parameter analysis in the differential diagnosis of large cell anemia disease[J]. Jilin Med J, 2022, 43( 3): 793- 795. DOI: 10.3969/j.issn.1004-0412.2022.03.087.汤俊峰, 卢爱微, 朱红梅, 等 血细胞多参数分析在大细胞性贫血疾病鉴别诊断中的应用[J]. 吉林医学, 2022, 43( 3): 793- 795. DOI: 10.3969/j.issn.1004-0412.2022.03.087. [13] KAUSHANSKY K, LICHTMAN MA, PRCHAL JT, et al. Willians Hematology. 9th Edition[M]. New York: McGraw-Hill Education, 2016: 481. [14] DENG L, LIU HY. Ultrastructural and morphological changes of red blood cells during extracorporeal circulation[J]. Chin J ECC, 2019, 17( 2): 117- 120. DOI: 10.13498/j.cnki.chin.j.ecc.2019.02.15.邓丽, 刘宏宇. 体外循环与红细胞损伤[J]. 中国体外循环杂志, 2019, 17( 2): 117- 120. DOI: 10.13498/j.cnki.chin.j.ecc.2019.02.15. [15] MURO N, BUJANDA L, SARASQUETA C, et al. Plasma levels of folate and vitamin B(12) in patients with chronic liver disease[J]. Gastroenterol Hepatol, 2010, 33( 4): 280- 287. DOI: 10.1016/j.gastrohep.2009.12.001. [16] YANG SS, YE ZL, LIU MY, et al. Associations of different serum folate forms with indices of nonalcoholic fatty liver disease and advanced fibrosis[J]. Obes Res Clin Pract, 2023, 17( 1): 58- 65. DOI: 10.1016/j.orcp.2023.01.004. [17] PIANO S, TONON M, VETTORE E, et al. Incidence, predictors and outcomes of acute-on-chronic liver failure in outpatients with cirrhosis[J]. J Hepatol, 2017, 67( 6): 1177- 1184. DOI: 10.1016/j.jhep.2017.07.008. [18] VARADARAJAN A, LAL D, KAPIL R, et al. Bone marrow dyspoiesis associated with severe refractory anaemia in liver cirrhosis[J]. Frontline Gastroenterol, 2021, 12( 1): 39- 43. DOI: 10.1136/flgastro-2019-101350. -



 PDF下载 ( 1037 KB)
PDF下载 ( 1037 KB)

 下载:
下载: